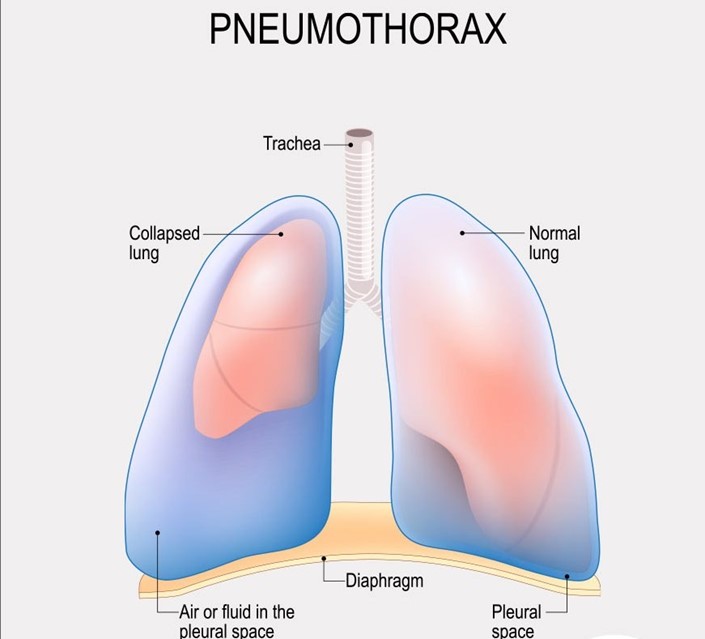
A nurse is assessing a client who has a pneumothorax with a chest tube in place. For which of the following findings should the nurse notify the provider?
Crepitus in the area above and surrounding the insertion site
Bubbling of the water in the water seal chamber with exhalation
Eyelets are not visible
Movement of the trachea toward the unaffected side
The Correct Answer is D
Choice A Reason: This is incorrect because crepitus in the area above and surrounding the insertion site is not a serious finding that requires notification of the provider. Crepitus is a crackling sensation that occurs when air leaks into the subcutaneous tissue. It is usually harmless and resolves on its own.
Choice B reason: This is incorrect because bubbling of the water in the water seal chamber with exhalation is a normal finding that indicates that air is being removed from the pleural space. Bubbling should stop when the pneumothorax is resolved.
Choice C Reason: This is incorrect because eyelets are not visible is not a serious finding that requires notification of the provider. Eyelets are small holes at the end of the chest tube that allow air and fluid to drain from the pleural space. They are usually covered by a dressing and may not be visible.
Choice D Reason: This is correct because movement of the trachea toward the unaffected side is a serious finding that indicates a tension pneumothorax, which is a life-threatening condition that occurs when air accumulates in the pleural space and causes pressure on the mediastinum. The nurse should notify the provider immediately and prepare for needle decompression or chest tube insertion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: Cause of the burn is not the nurse's priority when assessing the severity of the client's burns. The cause of the burn may indicate the type and duration of exposure, such as thermal, chemical, electrical, or radiation, which can affect the depth and extent of injury. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice B Reason: Age of the client is not the nurse's priority when assessing the severity of the client's burns. The age of the client may influence the response to burn injury, such as healing time, infection risk, and fluid requirements.
However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice C Reason: Associated medical history is not the nurse's priority when assessing the severity of the client's burns. The associated medical history may affect the outcome and prognosis of burn injury, such as pre-existing conditions, medications, or allergies. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Location of the burn is the nurse's priority when assessing the severity of the client's burns. The location of the burn can indicate the potential for life-threatening complications, such as airway obstruction, inhalation injury, or impaired circulation. The nurse should assess for signs and symptoms of respiratory distress, such as stridor, wheezes, or cyanosis, and prepare for endotracheal intubation if needed. The nurse should also monitor for signs and symptoms of compartment syndrome, such as pain, pallor, paresthesia, pulselessness, or paralysis, and report any findings to the provider. The location of the burn can also affect the functional and cosmetic outcomes, such as vision loss, facial disfigurement, or joint contractures. The nurse should provide appropriate wound care, pain management, and rehabilitation as prescribed. Assessing for location of burn is essential to prevent further injury and preserve vital functions.
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because respiratory alkalosis is characterized by a high pH and a low PaCO2, indicating that the client is hyperventilating and losing too much carbon dioxide.
Choice B Reason: This is incorrect because metabolic acidosis is characterized by a low pH and a low bicarbonate level, indicating that the client has an excess of metabolic acids or a loss of base.
Choice C Reason: This is incorrect because metabolic alkalosis is characterized by a high pH and a high bicarbonate level, indicating that the client has an excess of base or a loss of metabolic acids.
Choice D Reason: This is correct because respiratory acidosis is characterized by a low pH and a high PaCO2, indicating that the client is hypoventilating and retaining too much carbon dioxide.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
