A mother brings her 3-week-old son to the clinic because he is vomiting "all the time." In performing a physical assessment, the nurse notes that the infant has poor skin turgor, has lost 20% of his birth weight, and has a small palpable oval-shaped mass in his abdomen. Which intervention should the nurse implement first?
Initiate a prescribed IV for parenteral fluid.
Feed the infant 3 ounces of Isomil.
Give the infant 5% dextrose in water orally.
Insert a nasogastric tube for feeding.
The Correct Answer is A
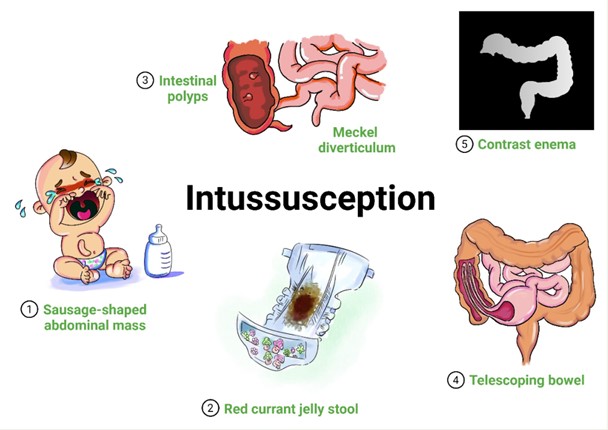
The presenting symptoms of the infant, including persistent vomiting, poor skin turgor, significant weight loss, and a palpable abdominal mass, indicate a potential serious condition that requires immediate attention. These findings may suggest dehydration, malnutrition, and the presence of an abdominal mass that could be causing gastrointestinal obstruction or other underlying pathology.
Initiating a prescribed IV for parenteral fluid is the priority intervention to address the potential dehydration and fluid imbalance in the infant. This will help restore and maintain adequate hydration while further diagnostic evaluations and interventions are initiated.
Feeding the infant, giving 5% dextrose in water orally, or inserting a nasogastric tube for feeding should not be implemented as the first intervention in this case. It is important to stabilize the infant's fluid status before initiating oral feedings or other interventions to address the underlying cause of the symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A.Protect the site from getting wet during bathing. While it is important to avoid prolonged soaking, gentle rinsing with water is usually allowed. Complete avoidance of water is not typically necessary.Gentle bathing is important for hygiene.
B.Gently patting the skin dry after rinsing with water is a good practice as it helps to minimize friction and irritation to the sensitive skin. Rubbing or scrubbing the skin should be avoided.
C. Applying moisturizers to prevent dry skin can be beneficial for overall skin health, but it is important to consult with the healthcare team and follow specific instructions regarding the use of moisturizers during radiation therapy. Certain types of moisturizers or creams may interfere with the radiation treatment or cause skin irritation. Frequent application is not always necessary. Over-hydration can soften the skin and increase vulnerability.
D.Using a sponge to debride the affected area is not recommended during radiation therapy. The skin in the radiation treatment field is already sensitive and prone to damage, and using a sponge for debridement can further traumatize the skin. It is important to avoid any abrasive or rough handling of the treated skin.
Correct Answer is ["A","B","D"]
Explanation
A) Correct- Weighing the client and reporting any weight gain is a routine measurement that can be safely performed by the UAP. Weight gain can be an important indicator of fluid retention, a common issue in Cushing's syndrome.
B) Correct- Reporting any client complaints of pain or discomfort is important for monitoring the client's well-being and promptly addressing any potential issues.
C) Incorrect- Evaluating the client for sleep disturbances involves assessing the client's sleep patterns, quality, and potential disruptions. This requires nursing judgment and a deeper understanding of the client's condition and potential contributing factors, so it's not appropriate to delegate this task to the UAP.
D) Correct- Noting and reporting the client's food and liquid intake during meals and snacks is part of monitoring the client's nutritional status, which is an appropriate task for the UAP.
E) Incorrect- Assessing the client for weakness and fatigue involves a more comprehensive evaluation of the client's physical and physiological status, which requires nursing expertise. The nurse should directly assess and interpret these symptoms in the context of Cushing's syndrome to provide appropriate interventions.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
