A male client with acute kidney injury (AKI) is scheduled for his first hemodialysis treatment and asks the practical nurse (PN) how the treatments will be evaluated for effectiveness. The PN explains that blood samples will be collected for analysis. Which laboratory value should the PN explain as the best indicator of each hemodialysis?
Elevated potassium.
Decreased calcium.
Lowered hemoglobin.
Decreased creatinine.
The Correct Answer is D
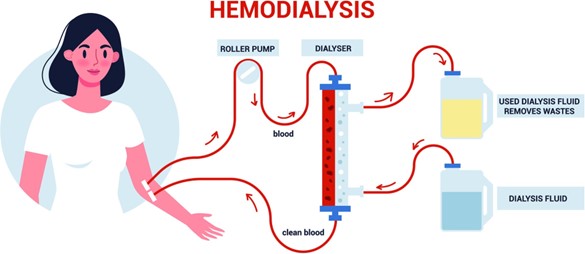
Hemodialysis is a procedure used to remove waste products and excess fluid from the blood when the kidneys are unable to function properly. One of the waste products that accumulate in the blood during kidney dysfunction is creatinine. Creatinine is a byproduct of muscle metabolism, and its levels in the blood are normally regulated and eliminated by the kidneys. In AKI, the kidneys are not able to effectively filter and eliminate creatinine, leading to elevated levels in the blood. Hemodialysis helps to remove excess creatinine from the blood, resulting in decreased creatinine levels.
A- Elevated potassium levels (hyperkalemia) are common in AKI and can be life-threatening. Hemodialysis helps to remove excess potassium from the blood, restoring normal levels.
However, the best indicator of the effectiveness of hemodialysis in managing hyperkalemia would be monitoring the potassium levels before and after the session rather than considering it as the "best" indicator.
B- Decreased calcium levels can occur in kidney dysfunction due to impaired activation of vitamin D and decreased absorption of calcium from the intestines. While hemodialysis can help restore calcium levels, it may not be the primary laboratory value used to evaluate the effectiveness of each session.
C- Lowered hemoglobin levels can be seen in AKI due to various factors, including decreased production of red blood cells and blood loss. Hemodialysis can help remove waste products and excess fluid, but it may not directly address the underlying causes of lowered hemoglobin levels.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
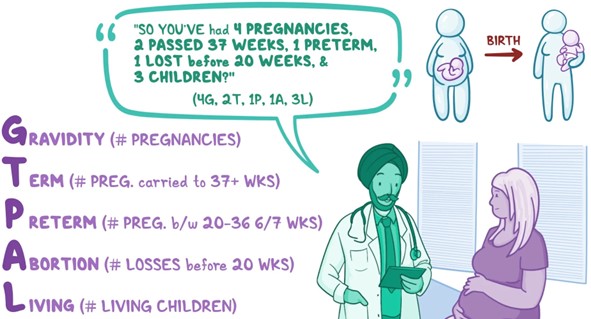
TPAL stands for Term, Premature, Abortion, and Living children, and it is used to document a client's obstetrical history.
In this case, the client has had a total of 5 pregnancies:
- Two pregnancies resulted in full-term (term) births, so the Term value is 2.
- Three pregnancies resulted in miscarriages during the first trimester (abortion), so the Abortion value is 3.
- The client has two living children, so the Living value is 2.
- There is no mention of any premature births, so the Premature value is 0.
Therefore, the appropriate documentation for this client's TPAL is Term 2, Premature 0, Abortion 3, and Living 2.
Correct Answer is D
Explanation
In cases of suspected child abuse, inconsistencies or discrepancies between the child's account of the injury and the caregiver's version are concerning. It raises questions about the credibility of the explanation provided by the caregiver and suggests a possible attempt to conceal the true cause of the injury. Such discrepancies may indicate that the injury was intentionally inflicted or that the child is being coerced or influenced to provide a false account.
While the other assessment findings may raise some level of concern, they are not as significant as the discrepancy between the child's and mother's versions of the injury:
A. "The mother refuses to answer questions about family history." While this behavior may raise some suspicion or cause for further investigation, it alone does not conclusively indicate child abuse. It may be related to other factors such as privacy concerns or cultural differences.
B. "The child has several abrasions on the chest and legs." While the presence of abrasions can be concerning, they alone do not provide sufficient evidence of child abuse. Children are prone to injuries and can obtain abrasions during normal play and activities.
C. "The child looks at the floor when answering the nurse's questions." This behavior may suggest shyness, anxiety, or discomfort, but it is not a definitive indicator of child abuse. Some children may exhibit such behaviors due to their personality or other factors unrelated to abuse. It is important to consider the child's overall behavior and communication patterns in conjunction with other assessment findings.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
