A client with Addison's disease becomes weak, confused, and dehydrated following the onset of an acute viral infection. The client's laboratory values include: sodium 129 mEq/L (129 mmol/L), glucose 54 mg/dl (2.97 mmol/L) and potassium 5.3 mEq/L (5.3 mmol/L).
When reporting the findings to the healthcare provider, the nurse anticipates a prescription for which intravenous medication?
Reference Ranges
- Sodium [Reference Range: Adult 136 to 145 mEq/L (136 to 145 mmol/L)
- Glucose (Reference Range: 0 to 50 years: 74 to 106 mg/dl. (4.1 to 5.9 mmol/L))
- Potassium [Reference Range: 3.5 to 5.0 mEq/L (3.5 to 5.0 mmol/L)
Broad spectrum antibiotic.
Regular insulin.
Hydrocortisone.
Potassium chloride.
The Correct Answer is C
The client with Addison's disease is experiencing weakness, confusion, and dehydration, which can be indicative of an adrenal crisis. The low sodium level (129 mEq/L) and low glucose level (54 mg/dl) further support this suspicion. An acute viral infection can trigger an adrenal crisis in individuals with Addison's disease.
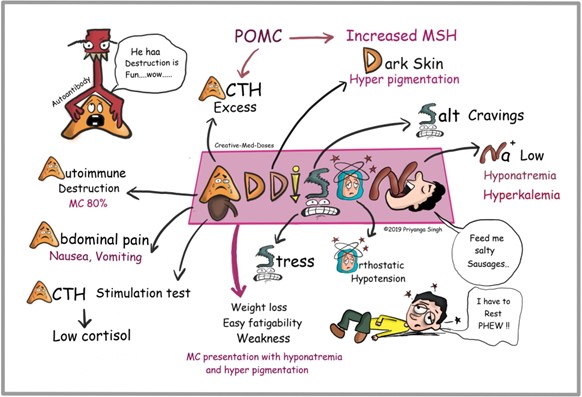
Intravenous hydrocortisone, a glucocorticoid, is the treatment of choice for managing an adrenal crisis. It helps to replenish cortisol levels and stabilize the client's condition.
Hydrocortisone helps in restoring the body's stress response and regulating electrolyte and glucose levels.
A broad-spectrum antibiotic may be necessary if there is evidence of a bacterial infection, but it does not directly address the symptoms associated with Addison's disease.
Regular insulin is used for managing high blood glucose levels in conditions such as diabetes, but in this case, the client has low glucose levels, so insulin is not the appropriate intervention.
Potassium chloride is a medication used to treat low potassium levels (hypokalemia), but the client's potassium level is within the reference range (5.3 mEq/L). Therefore, potassium chloride is not indicated in this situation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","D"]
Explanation
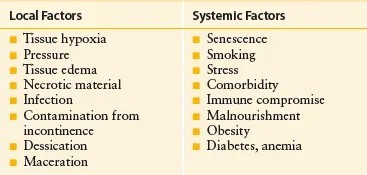
The age-related factors that may factor into this client's wound healing are: Decreased epidermal turnover: As people age, the turnover of skin cells decreases, resulting in slower wound healing. This can prolong the healing process and increase the risk of complications.
T-cell function decrease: The immune system's function, including T-cell function, tends to decline with age. T-cells play a crucial role in the immune response and wound healing. Decreased T-cell function can impair the body's ability to fight infection and promote efficient healing.
Insulin resistance and pigmentation changes are not directly age-related factors that impact wound healing. Insulin resistance is a condition related to impaired glucose metabolism and can affect wound healing in individuals with diabetes or other metabolic disorders, but it is not necessarily an age-related factor. Pigmentation changes are primarily cosmetic and do not directly affect the physiological processes involved in wound healing.
Correct Answer is A
Explanation
A.Tingling on the tongue or lips is an early sign of an allergic reaction to the contrast dye used during an intravenous pyelogram. This type of reaction can quickly progress to more severe symptoms, such as difficulty breathing and anaphylaxis, so it is crucial to recognize and respond to it promptly.
B. Episodes of shivering: Shivering is not typically an early sign of an allergic reaction to contrast dye. It might indicate a reaction to temperature or anxiety but is not as immediately concerning as symptoms of an allergic reaction.
C. Salty taste in the mouth: A salty or metallic taste is a common and benign side effect of the contrast dye and is not indicative of an adverse reaction.
D. Difficulty breathing: Difficulty breathing is a severe and later sign of an allergic reaction. By the time this symptom appears, the reaction has progressed and immediate intervention is necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
