A client with acute respiratory distress syndrome (ARDS) shows no improvement despite increases in concentration in oxygen administered. What intervention should the nurse attempt which may improve ventilation-perfusion matching?
Prone Position
Positioning supine with head elevated to 30-45 degrees
Infusion of Albumin
Transfusion of PRBC
The Correct Answer is A
A. Prone positioning involves turning the patient onto their abdomen to improve ventilation-perfusion matching by redistributing ventilation to the dorsal lung regions, where perfusion is typically better in ARDS patients.
B. Semi-recumbent positioning may be used to prevent aspiration and reduce the risk of VAP but is not as effective as prone positioning for improving V/Q matching.
C. Albumin infusion is not specific interventions for improving ventilation-perfusion matching in ARDS and should be considered based on other clinical indications.
D. Transfusion of packed red blood cells (PRBC) may be indicated in cases of severe anemia or hypoxemia due to inadequate oxygen-carrying capacity. However, it is not a primary intervention for improving ventilation-perfusion matching in ARDS
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
D. A drop in oxygen saturation may indicate inadequate oxygenation, which could be due to airway obstruction or retained secretions.
A. While audible expiratory wheezes may indicate airway obstruction or secretions, they do not necessarily indicate the need for suctioning in a patient receiving mechanical ventilation.
B. An elevated respiratory rate may suggest increased work of breathing, which could be due to retained secretions or airway obstruction. However, an elevated respiratory rate alone may not always indicate the need for suctioning.
C. The timing of the last suctioning episode is an important consideration when determining the need for suctioning. However, it should not be the sole indicator for when to suction.
Correct Answer is B
Explanation
B This maneuver, called the Valsalva maneuver, can sometimes help to restore normal heart rhythm in cases of SVT. It involves blowing forcefully into a syringe or performing a similar action that increases intra-abdominal pressure, which can stimulate the vagus nerve and help to slow down the heart rate.
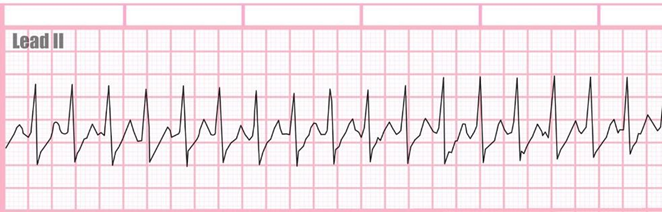
A Defibrillation is a treatment used for life-threatening cardiac arrhythmias, particularly ventricular fibrillation or pulseless ventricular tachycardia. It involves delivering a therapeutic dose of electrical energy to the heart with a device called a defibrillator.
C Drawing troponin levels may be appropriate if there is suspicion of myocardial infarction as the cause of chest palpitations or if there are other symptoms suggestive of acute coronary syndrome. However, in the context of SVT presenting with chest palpitations and a racing heart, the priority is to address the arrhythmia first
D Amiodarone is an antiarrhythmic medication used to treat various types of cardiac arrhythmias, including ventricular and supraventricular arrhythmias. While it can be effective in certain cases of SVT, it is not typically the first-line treatment or the immediate next step in managing SVT in the emergency department.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
