A client with a cervical spinal injury (C7) is experiencing autonomic dysreflexia. The nurse should first assess the client for which precipitating factor?
An acutely distended bladder.
Profuse forehead diaphoresis.
Skeletal traction misalignment.
A severe pounding headache.
The Correct Answer is A
A. One of the most common triggers is a distended bladder. When the bladder becomes full, it sends signals to the spinal cord, but due to the injury, these signals are unable to pass beyond the level of injury. This results in uncontrolled sympathetic activation, leading to symptoms such as hypertension, sweating, and headache.
B. Forehead diaphoresis, or sweating, is a potential symptom of autonomic dysreflexia. However, it is more of a consequence rather than a precipitating factor. It occurs as a result of sympathetic nervous system activation in response to the triggering stimulus.
C. Skeletal traction misalignment is not a common precipitating factor for autonomic dysreflexia. Autonomic dysreflexia is typically triggered by stimuli related to visceral or autonomic reflexes, such as bladder distention or bowel impaction, rather than mechanical issues like traction misalignment.
D. A severe pounding headache can occur as a symptom of autonomic dysreflexia, but it is not the primary precipitating factor. The headache is a result of the sudden increase in blood pressure that occurs during autonomic dysreflexia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. This choice involves culturing a sputum sample collected from the patient to identify the presence of Mycobacterium tuberculosis, the bacterium that causes tuberculosis. A positive result confirms the diagnosis of TB.
B. Hemoccult tests are used to detect hidden (occult) blood in stool samples. While hemoptysis (coughing up blood) can be a symptom of TB, a hemoccult test is not specific for TB diagnosis. It is more commonly used in detecting gastrointestinal bleeding.
C. Imaging studies like chest x-ray or CT scans can reveal abnormalities in the lungs suggestive of TB, such as infiltrates, cavitations, or lymph node enlargement. While these tests can support the diagnosis, they are not definitive on their own.
D. The PPD skin test is a common screening tool for TB exposure. It detects the presence of a delayed hypersensitivity reaction to proteins derived from Mycobacterium tuberculosis. A positive PPD indicates exposure to TB but does not confirm active disease.
Correct Answer is B
Explanation
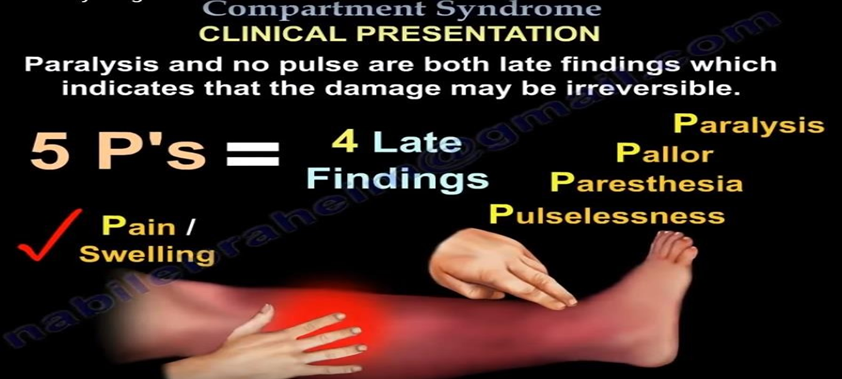
B. An increase in pain after cast placement could indicate complications such as compartment syndrome, which is a serious condition that occurs when increased pressure within a confined space (such as the area within the cast) compromises circulation and tissue perfusion. Assessing the radial pulse volume on the affected arm is crucial to evaluate perfusion distal to the fracture site.
A. Distraction technique may help manage the client's pain but does not address the underlying cause of the pain increase, which could be related to compromised circulation.
C. Analgesics relieve pain but do not address the immediate limb threatening issue at hand.
D. Measuring blood pressure is not directly related to assessing circulation distal to the fracture site.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
