The child is a 2-year-old who fell into a pool. He was retrieved from the pool by a family member but was not breathing. The family member started CPR, and the ambulance brought him to the hospital.
What factors are important in determining the level of hypoxemia that the child may have experienced during the submersion?
Select all that apply.
Temperature of water
The weight of the child
Oxygen concentration of the ambient air
Whether or not anyone witnessed the fall into the pool
The amount of time the child was submerged
Correct Answer : A,E
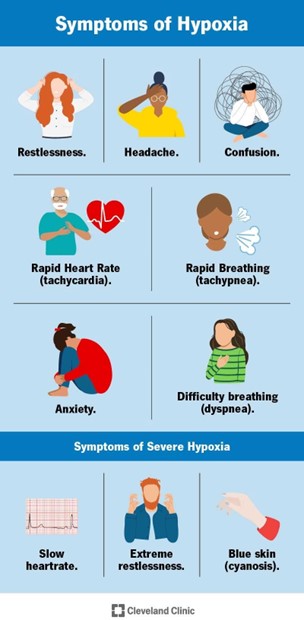
The level of hypoxemia that the child may have experienced during the submersion depends on several factors, but the most important ones are:
- The **temperature of water**: Cold water can induce a diving reflex, which lowers the heart rate and oxygen consumption, and may protect the brain from hypoxic injury¹². Cold water can also cause laryngospasm, which prevents water aspiration but also impairs gas exchange.
- The **amount of time the child was submerged**: The longer the submersion, the more severe the hypoxemia and the higher the risk of brain damage and death. The survival rate decreases significantly after 5 minutes of submersion³.
The other factors are less relevant or not directly related to the level of hypoxemia:
- The **weight of the child**: This may affect the buoyancy and the ability to float or swim, but not the oxygen consumption or gas exchange during submersion¹.
- The **oxygen concentration of the ambient air**: This may affect the pre-submersion oxygen saturation, but not the rate of oxygen depletion or gas exchange during submersion¹.
- The **witnessing of the fall into the pool**: This may affect the time to rescue and resuscitation, but not the level of hypoxemia during submersion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","D"]
Explanation
They are needed to remove the saline lock safely and prevent bleeding or infection. The PN should wear exam gloves to protect themselves and the client from contamination, apply a small gauze pad over the insertion site, and secure it with paper tape after removing the saline lock.
Correct Answer is ["B","D"]
Explanation
A) Incorrect - Providing a regular diet tray is important for the client's nutritional needs, but it is not as urgent as assessing vital signs or administering Albuterol in response to the client's acute symptoms.
B) Correct- This action is a priority after any assessment or intervention. Vital signs provide important information about the client's overall condition, including heart rate, blood pressure, respiratory rate, and oxygen saturation.
C) Incorrect - Applying oxygen is important, but its priority depends on the client's vital signs and oxygen saturation, which should be assessed first.
D) Correct- Administering Albuterol as ordered is crucial for addressing the client's acute breathing difficulty. Albuterol is a bronchodilator that helps alleviate asthma symptoms, and timely administration is essential.
E) Incorrect - Performing a pulmonary function test is valuable for assessing lung function, but it's not an immediate concern compared to addressing the client's breathing difficulty.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
