The nurse is caring for a client recovering from an esophagogastroduodenoscopy (EGD). Which of the following client symptoms would require further nursing assessment?
Thirst
Sore throat
Abdominal distention
Drowsiness
The Correct Answer is C
Choice A Reason:
Thirst is a common and expected symptom after an EGD, especially if the client has been fasting before the procedure. It does not typically indicate a complication and can be managed by gradually reintroducing fluids as tolerated. Therefore, thirst does not require further nursing assessment beyond routine post-procedure care.
Choice B Reason:
A sore throat is also a common symptom following an EGD. The procedure involves passing an endoscope through the throat, which can cause temporary irritation and discomfort. This symptom usually resolves on its own within a few days and does not indicate a serious complication. Therefore, a sore throat does not require further nursing assessment beyond providing comfort measures such as lozenges or warm saltwater gargles.
Choice C Reason:
Abdominal distention is a concerning symptom that requires further nursing assessment. It can indicate complications such as perforation, bleeding, or infection following the EGD. Perforation of the gastrointestinal tract is a rare but serious complication that can lead to peritonitis and sepsis if not promptly addressed. Therefore, any signs of abdominal distention should be reported to the provider immediately for further evaluation and intervention.
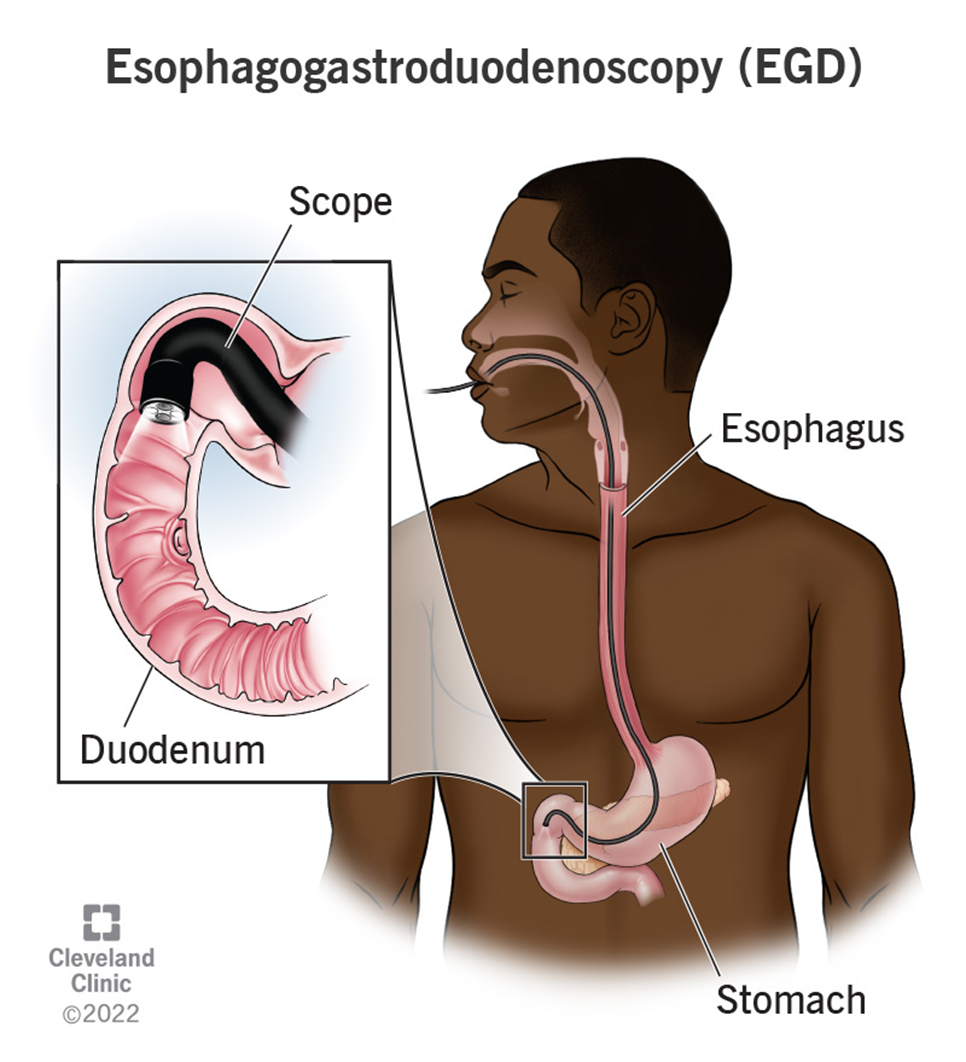
Choice D Reason:
Drowsiness is a common side effect of the sedatives used during the EGD procedure. It is expected that the client may feel drowsy or sleepy for a few hours after the procedure as the sedative wears off. This symptom does not typically require further nursing assessment unless it persists for an unusually long time or is accompanied by other concerning symptoms such as difficulty breathing or altered mental status.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
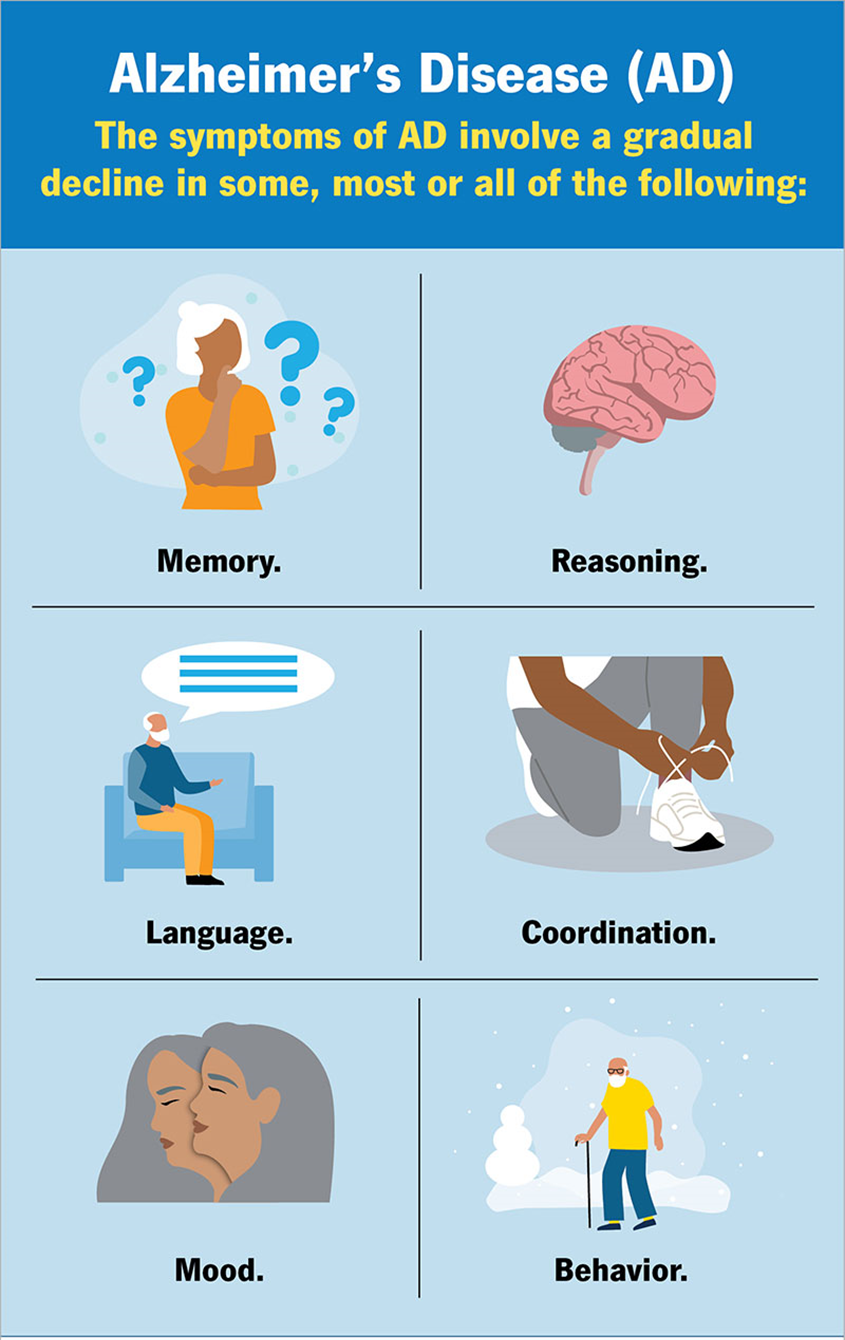
Correct Answer is D
Explanation
Choice A Reason:
Low oxygen saturation is not a common side effect of donepezil. Donepezil is a cholinesterase inhibitor used to treat symptoms of Alzheimer’s disease by increasing the levels of acetylcholine in the brain. While it can have various side effects, respiratory issues like low oxygen saturation are not typically associated with this medication. Therefore, monitoring for low oxygen saturation is not a primary concern for patients starting donepezil.
Choice B Reason:
High blood pressure is also not a common side effect of donepezil. The medication primarily affects the central nervous system and does not typically cause significant changes in blood pressure. While it is always important to monitor a patient’s overall health, high blood pressure is not a side effect specifically linked to donepezil use. Therefore, it is not a primary focus for monitoring in this context.
Choice C Reason:
Elevated body temperature is not commonly associated with donepezil. The side effects of donepezil are more likely to involve gastrointestinal issues such as nausea, vomiting, and diarrhea, as well as muscle cramps and fatigue. Elevated body temperature is not a typical reaction to this medication, so it is not a primary concern for monitoring.
Choice D Reason:
Low pulse rate, or bradycardia, is a known side effect of donepezil. Donepezil can increase the levels of acetylcholine, which can affect the heart’s electrical conduction system and lead to a slower heart rate. This can be particularly concerning in elderly patients or those with pre-existing heart conditions. Therefore, it is crucial for the nurse to teach the family to monitor the client’s pulse rate regularly and report any significant decreases to the healthcare provider.
Correct Answer is A
Explanation
Choice A: He is NPO until the speech-language pathologist performs a swallowing evaluation.
This is the most appropriate response. NPO stands for “nil per os,” which means nothing by mouth. After a stroke, it is crucial to assess the patient’s ability to swallow safely to prevent aspiration, which can lead to pneumonia and other complications. A speech-language pathologist is trained to evaluate swallowing function and determine the safest diet for the patient. Until this evaluation is completed, the patient should not consume any food or liquids.
Choice B: Be sure to sit him up when you are feeding him to make him feel more natural.
While sitting the patient up during feeding is important to reduce the risk of aspiration, it is not sufficient on its own. Without a proper swallowing evaluation, feeding the patient could still pose significant risks. Therefore, this choice is not the most appropriate response.
Choice C: You may give him a full-liquid diet, but please avoid solid foods until he gets stronger.
A full-liquid diet might seem like a safer option, but without a swallowing evaluation, there is still a risk of aspiration. The patient’s ability to handle even liquids needs to be assessed by a professional before any oral intake is allowed.
Choice D: Just be sure to add some thickener in his liquids to prevent choking and aspiration.
Thickening liquids can help manage dysphagia, but this should only be done after a swallowing evaluation has determined the appropriate consistency. Administering thickened liquids without an evaluation could still result in aspiration if the patient has severe swallowing difficulties.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
