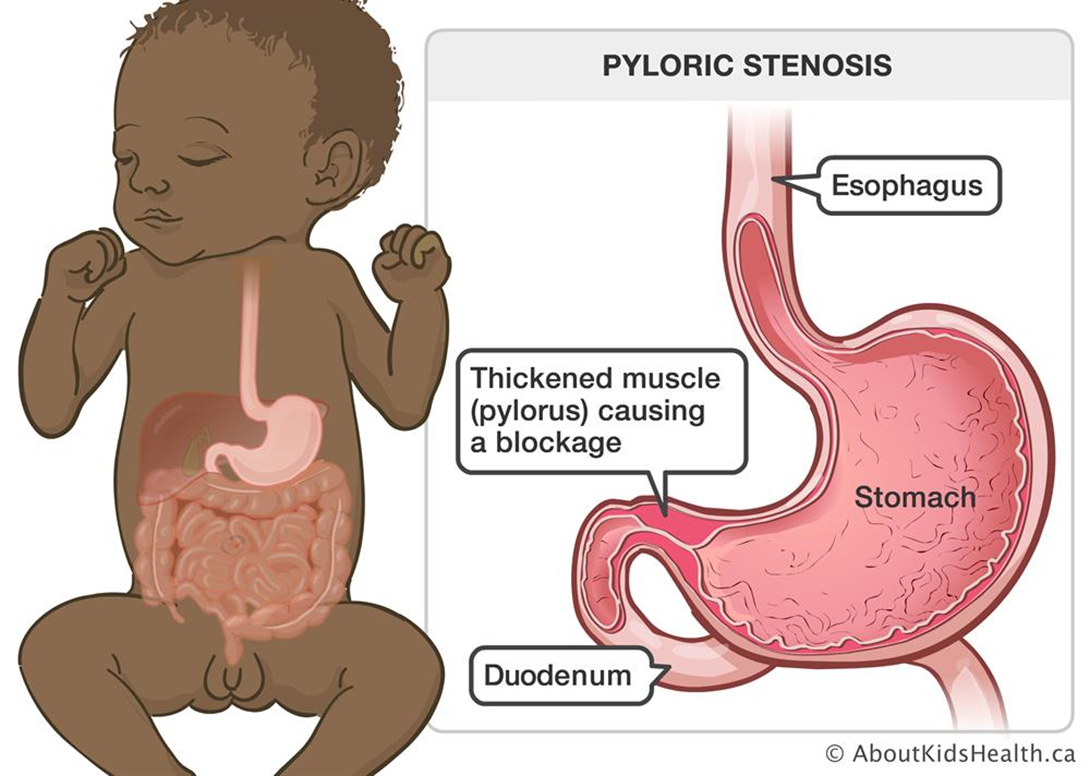
A 6-week-old infant with pyloric stenosis is scheduled for a pyloromyotomy. Which pre-operative nursing action has the highest priority?
Mark an outline of the "olive-shaped" mass in the right epigastric area.
Instruct parents regarding care of the incisional area.
Monitor amount of intake and infant's response to feedings.
Initiate a continuous infusion of IV fluids per prescription.
The Correct Answer is D
Choice A reason: Marking an outline of the "olive-shaped" mass in the right epigastric area is not a priority nursing action. The mass is caused by hypertrophy of the pyloric sphincter, which obstructs gastric emptying and causes projectile vomiting. The mass may not be palpable in all cases.
Choice B reason: Instructing parents regarding care of the incisional area is a post-operative nursing action, not a pre-operative one. The parents will need to learn how to keep the incision clean and dry, monitor for signs of infection, and administer pain medication as prescribed.
Choice C reason: Monitoring amount of intake and infant's response to feedings is important, but not the highest priority. The infant may have difficulty feeding due to nausea, vomiting, and abdominal pain.
Choice D reason: This is the correct answer because initiating a continuous infusion of IV fluids per prescription is essential to prevent dehydration and electrolyte imbalance in the infant. The infant may have significant fluid loss due to vomiting and poor intake.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","C","D"]
Explanation
Choice A reason: This is a correct answer because continuing to monitor the client for signs of an infection is important to detect any recurrence or complication of MRSA infection. MRSA is a type of bacteria that is resistant to many antibiotics and can cause serious skin, soft tissue, bone, joint, or bloodstream infections. The nurse should assess the client's vital signs, wound appearance, pain level, and laboratory results.
Choice B reason: This is not a correct answer because calling the healthcare provider for a prescription for linezolid is not necessary unless the client has an active MRSA infection that requires treatment. Linezolid is an antibiotic that can be used to treat MRSA infections, but it has potential side effects and interactions that need to be considered. The nurse should not prescribe or administer antibiotics without a valid order.
Choice C reason: This is a correct answer because collecting multiple sets of blood cultures for MRSA screening is important to identify any asymptomatic bacteremia or sepsis that could result from MRSA infection. MRSA can enter the bloodstream through wounds, catheters, or surgical sites and cause life-threatening complications such as endocarditis, osteomyelitis, or pneumonia. The nurse should obtain blood samples from different sites and times and send them to the laboratory for analysis.
Choice D reason: This is a correct answer because placing the client on contact transmission precautions is important to prevent the spread of MRSA to other clients, staff, or visitors. Contact transmission precautions include wearing gloves and gowns when entering the client's room, using dedicated or disposable equipment, and performing hand hygiene before and after contact with the client or their environment.
Choice E reason: This is not a correct answer because obtaining a sputum specimen for culture and sensitivity is not relevant to the client's history of MRSA wound infection. Sputum culture and sensitivity is a test that can be used to diagnose respiratory infections caused by bacteria, fungi, or viruses. The nurse should only obtain a sputum specimen if the client has signs or symptoms of a respiratory infection, such as cough, fever, chest pain, or dyspnea.
Correct Answer is D
Explanation
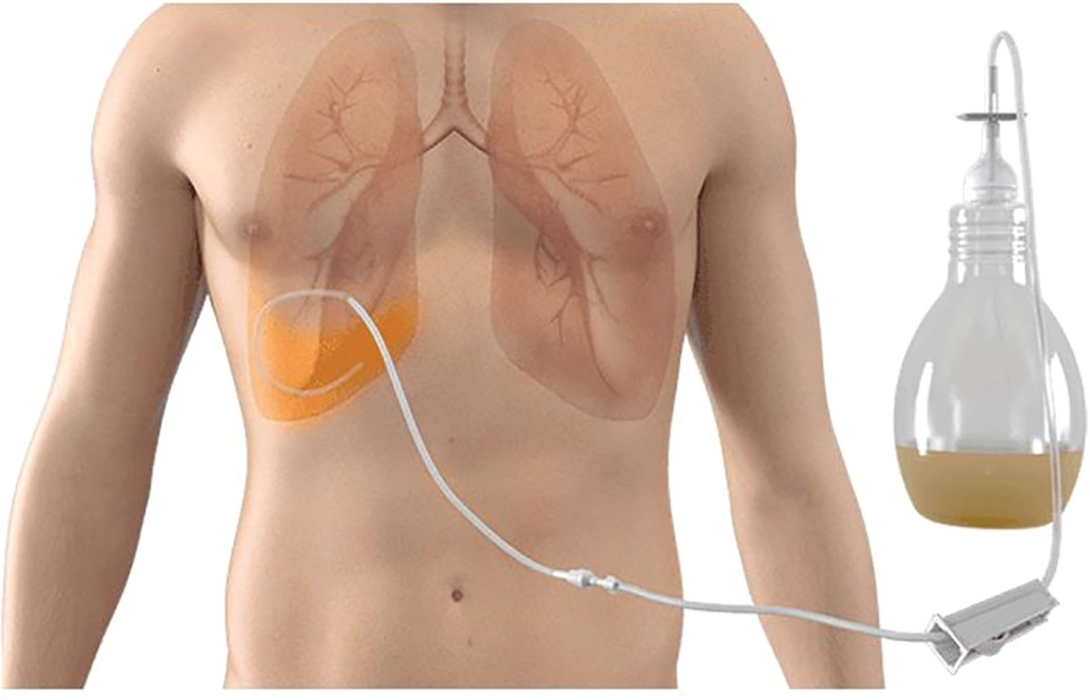
Choice A reason: Securing chest tube to the stretcher for transport is not the most important action for the nurse to take. Chest tube is a device that drains air or fluid from the pleural space or mediastinum after surgery or trauma. Securing chest tube to the stretcher can prevent accidental dislodgement or kinking of the tube during transport, but it is not as crucial as maintaining proper drainage.
Choice B reason: Administering PRN pain medication prior to transport is not the most important action for the nurse to take. Pain medication is a drug that relieves pain by blocking pain signals or reducing inflammation. Administering pain medication prior to transport can improve comfort and reduce anxiety for the client, but it is not as urgent as preventing complications.
Choice C reason: Marking the amount of chest drainage on the container is not the most important action for the nurse to take. Chest drainage is the fluid or air that collects in the chest tube container after being drained from the pleural space or mediastinum. Marking the amount of chest drainage on the container can help monitor fluid balance and detect excessive bleeding or leakage, but it is not as vital as ensuring proper drainage.
Choice D reason: This is the correct answer because keeping chest tube container below the site of insertion is the most important action for the nurse to take. Chest tube container is a device that collects air or fluid from the chest tube and maintains negative pressure in the pleural space or mediastinum. Keeping chest tube container below the site of insertion can prevent backflow of air or fluid into the chest cavity and maintain adequate drainage. If the chest tube container is raised above the site of insertion, it can cause tension pneumothorax, which is a life-threatening condition that occurs when air accumulates in the pleural space and compresses the lung and heart.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
