A patient who is hypotensive is receiving dopamine, an adrenergic agonist IV at the rate of 6 mcg/kg/min. Which intervention should the nurse implement when administering this medication?
Implement seizure precautions.
Monitor serum potassium frequently.
Ensure pump accuracy to prevent toxicity.
Measure urinary output every hour.
The Correct Answer is C
Choice A reason: This is incorrect because seizure precautions are not indicated for dopamine administration. Dopamine does not lower the seizure threshold or cause convulsions.
Choice B reason: This is incorrect because monitoring serum potassium frequently is not necessary for dopamine administration. Dopamine does not affect potassium levels or cause hyperkalemia or hypokalemia.
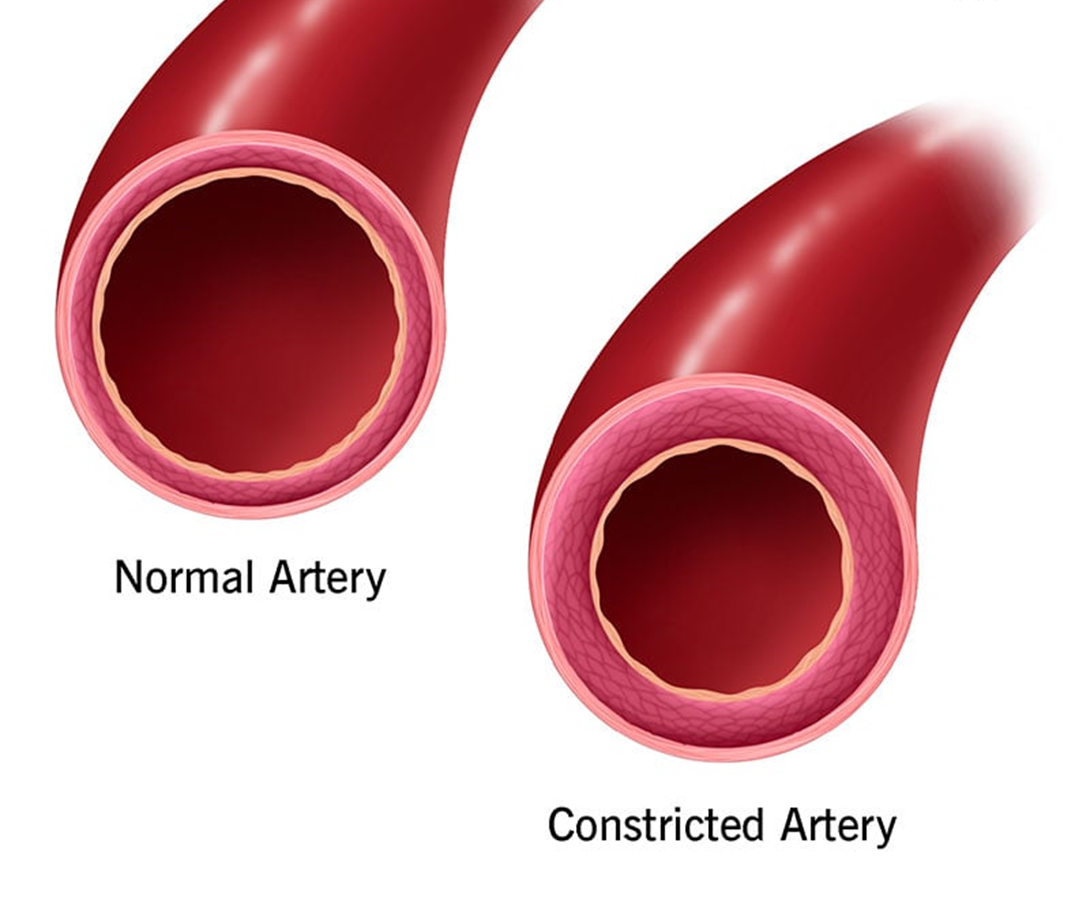
Choice C reason: This is correct because ensuring pump accuracy to prevent toxicity is essential for dopamine administration. Dopamine is a potent vasoconstrictor that can cause tissue necrosis, gangrene, and hypertension if overdosed.
Choice D reason: This is incorrect because measuring urinary output every hour is not sufficient for dopamine administration. Dopamine can cause oliguria or anuria due to renal vasoconstriction and decreased renal perfusion. The nurse should monitor urine output continuously and report any decrease to the provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["1"]
Explanation
To calculate how many mL/hr the nurse should program the infusion pump, we need to use the following formula:
mL/hr = (units/hr) / (units/mL)
where units/hr is the prescribed dose of insulin per hour, and units/mL is the concentration of insulin in the IV solution.
In this case, we are given that:
units/hr = 1 unit (the usual starting dose for IV insulin)
units/mL = 100 units / 100 mL = 1 unit/mL
Plugging these values into the formula, we get:
mL/hr = (1 unit/hr) / (1 unit/mL)
mL/hr = 1 mL/hr
Therefore, the nurse should program the infusion pump to deliver 1 mL/hr.
Correct Answer is D
Explanation
Choice A reason: Client’s healthcare power of attorney. This is not the first information that the nurse should provide, as it does not address the current situation or problem of the client. The healthcare power of attorney is a legal document that designates who can make medical decisions for the client if they are unable to do so themselves.
Choice B reason: Currently prescribed medications. This is not the first information that the nurse should provide, as it does not address the current situation or problem of the client. The currently prescribed medications are a part of the background information that can help explain the client’s medical history and potential causes of confusion.
Choice C reason: Fall at home as reason for admission. This is not the first information that the nurse should provide, as it does not address the current situation or problem of the client. The fall at home is a part of the background information that can help explain the client’s reason for admission and potential injuries.
Choice D reason: Increasing confusion of the client. This is the first information that the nurse should provide, as it addresses the current situation or problem of the client. The increasing confusion of the client is a part of the assessment information that can help identify the urgency and severity of the issue and guide further interventions.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
