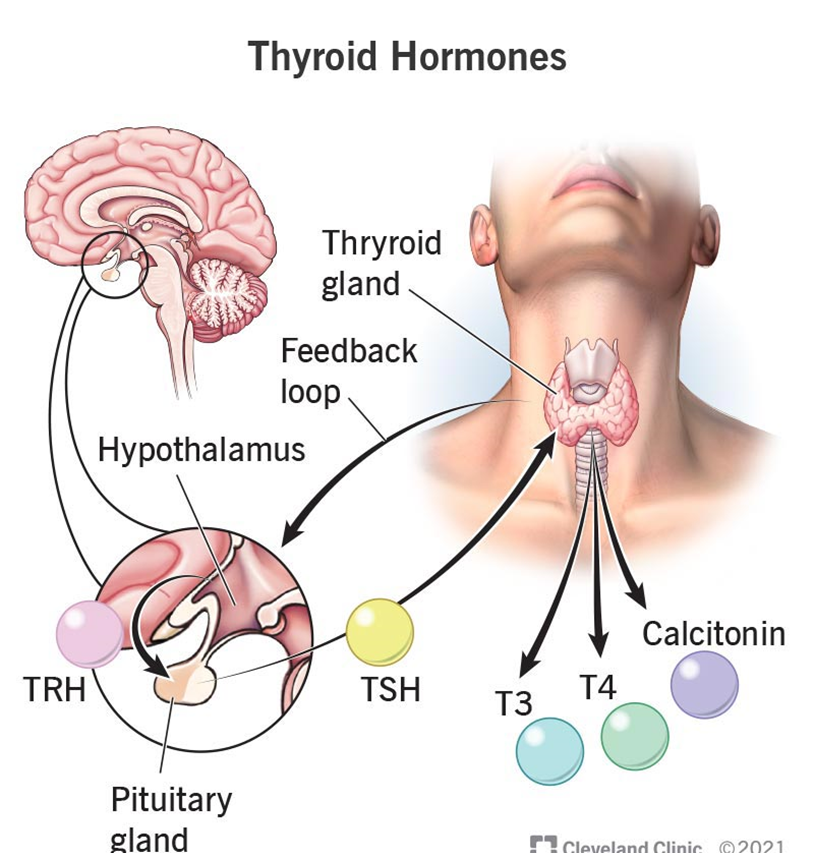
A nurse is reviewing laboratory results and notes that a client has an elevated thyroid-stimulating hormone (TSH) level. Which of the following assessment findings would the nurse expect?
Increased thirst, increased urine output, and weight loss
Fatigue, constipation, weight gain
Anxiety, unintended weight loss, palpitations
Shakiness, sweating, nausea
The Correct Answer is B
Choice A reason: Increased Thirst, Increased Urine Output, and Weight Loss
Increased thirst, increased urine output, and weight loss are symptoms commonly associated with diabetes mellitus, particularly uncontrolled diabetes. These symptoms occur due to the body’s attempt to eliminate excess glucose through urine, leading to dehydration and subsequent weight loss. However, these symptoms are not typically associated with elevated TSH levels, which indicate hypothyroidism.
Choice B reason: Fatigue, Constipation, Weight Gain
Fatigue, constipation, and weight gain are classic symptoms of hypothyroidism2. When the thyroid gland is underactive, it produces insufficient thyroid hormones, leading to a slowdown in the body’s metabolism. This results in fatigue, weight gain, and constipation, among other symptoms. Elevated TSH levels are a compensatory response by the pituitary gland to stimulate the thyroid to produce more hormones, confirming hypothyroidism.
Choice C reason: Anxiety, Unintended Weight Loss, Palpitations
Anxiety, unintended weight loss, and palpitations are symptoms typically associated with hyperthyroidism, not hypothyroidism. Hyperthyroidism occurs when the thyroid gland produces excessive thyroid hormones, leading to an accelerated metabolism. This results in symptoms such as weight loss, increased heart rate (palpitations), and anxiety. Elevated TSH levels would not be expected in hyperthyroidism; instead, TSH levels would be low due to negative feedback from high thyroid hormone levels.
Choice D reason: Shakiness, Sweating, Nausea
Shakiness, sweating, and nausea can be symptoms of various conditions, including hypoglycemia (low blood sugar), anxiety, or panic attacks. These symptoms are not specific to thyroid dysfunction and are not typically associated with elevated TSH levels. Hypothyroidism, indicated by high TSH levels, usually presents with symptoms related to a slowed metabolism, such as fatigue and weight gain, rather than shakiness and sweating.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The correct answer is a) Serum potassium levels.
Choice A reason:
Serum potassium levels are crucial to monitor in clients with hypervolemia, ketoacidosis, and metabolic acidosis. Potassium imbalances are common in these conditions due to shifts between intracellular and extracellular compartments. In diabetic ketoacidosis (DKA), for example, insulin deficiency and acidosis cause potassium to move out of cells, leading to hyperkalemia. However, once treatment with insulin begins, potassium shifts back into cells, which can cause hypokalemia. Both hyperkalemia and hypokalemia can have serious cardiac implications, making it essential to monitor and manage potassium levels closely.
Choice B reason:
Serum calcium levels are important for overall health, but they are not the primary concern in the context of hypervolemia, ketoacidosis, and metabolic acidosis. While calcium imbalances can occur, they are less common and less immediately life-threatening compared to potassium imbalances. Monitoring calcium is still necessary, but it does not require the same level of immediate intervention.
Choice C reason:
Serum sodium levels are also important to monitor, especially in conditions like hypervolemia where fluid balance is disrupted. However, sodium imbalances are typically managed through fluid management and do not pose the same immediate risk as potassium imbalances in the context of ketoacidosis and metabolic acidosis. Hyponatremia or hypernatremia can cause neurological symptoms, but these are generally less acute compared to the cardiac risks associated with potassium imbalances.
Choice D reason:
Blood urea nitrogen (BUN) levels provide information about kidney function and hydration status. Elevated BUN can indicate dehydration or renal impairment, which are relevant in the context of hypervolemia and ketoacidosis. However, BUN levels do not require the same level of immediate intervention as potassium levels. Monitoring BUN is important for overall management but is not the primary concern in acute settings.
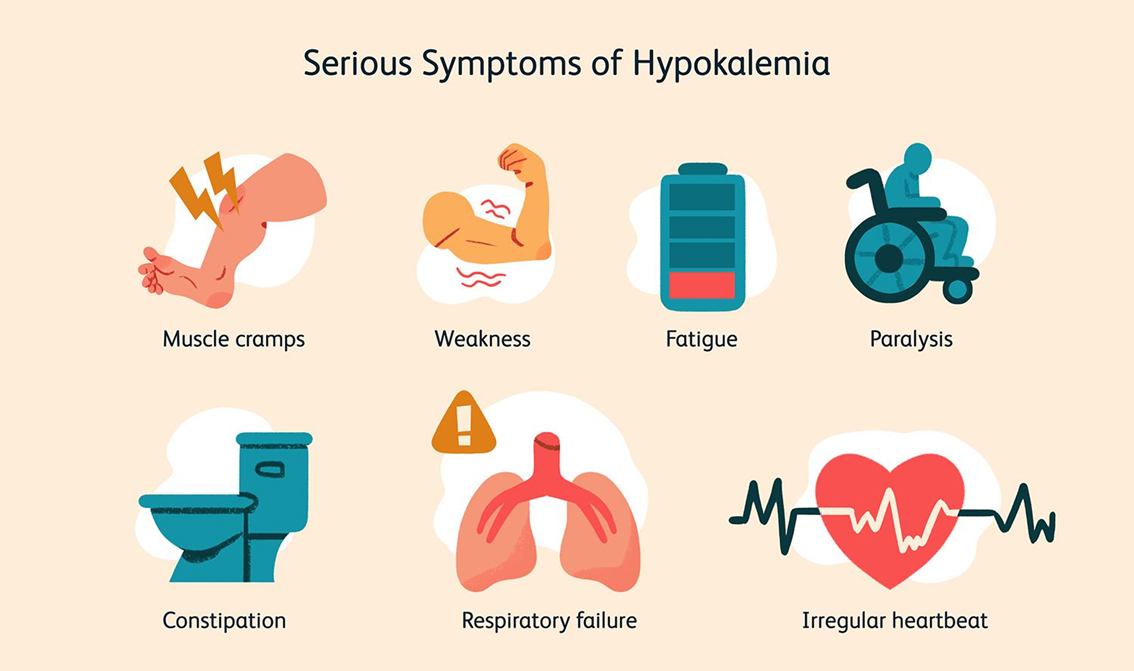
Correct Answer is D
Explanation
Choice A reason: Hypertension is not directly caused by hypokalemia. While potassium levels can influence blood pressure, hypokalemia is more critically associated with cardiac issues rather than hypertension alone.
Choice B reason: Ketosis is a metabolic state resulting from the body burning fat for fuel instead of carbohydrates. It is not directly related to hypokalemia. Hypokalemia does not cause ketosis, and monitoring for ketosis in a client with hypokalemia is not a priority.
Choice C reason: Insulin resistance is a condition where the body’s cells do not respond properly to insulin. While potassium levels can affect insulin secretion and action, hypokalemia is not primarily associated with insulin resistance. Therefore, it is not the main concern for a nurse monitoring a client with hypokalemia.
Choice D reason: Cardiac arrhythmias are a significant concern in clients with hypokalemia. Potassium is crucial for proper cardiac function, and low levels can lead to abnormal heart rhythms. This is why monitoring for cardiac arrhythmias is essential in clients with hypokalemia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
