A client is on a ventilator. Alarms are sounding, indicating an increase in peak airway pressure. The nurse assesses first for what?
Malfunction of the alarm button.
A cut or slice in the tubing from the ventilator.
Higher than normal endotracheal cuff pressure.
A kink in the ventilator tubing.
The Correct Answer is D
Choice A Reason:
Malfunction of the alarm button is unlikely to be the cause of increased peak airway pressure. The alarm is designed to alert the nurse to a problem with the ventilator or the patient’s airway, not to malfunction itself. Therefore, this is not the first thing the nurse should assess.
Choice B Reason:
A cut or slice in the tubing from the ventilator could cause a loss of pressure or air leak, but it would not typically result in increased peak airway pressure. Instead, it would likely cause a decrease in pressure and potentially trigger a different alarm.
Choice C Reason:
Higher than normal endotracheal cuff pressure can contribute to increased peak airway pressure. However, it is not the most immediate concern compared to a kink in the tubing, which can completely obstruct airflow and rapidly compromise the patient’s ventilation.
Choice D Reason:
A kink in the ventilator tubing is a common and immediate cause of increased peak airway pressure. It obstructs the flow of air, leading to a buildup of pressure in the system. This is the first thing the nurse should assess and correct to ensure the patient is receiving adequate ventilation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason: No change to the heparin rate is not appropriate in this scenario. The normal range for PTT is generally between 25 to 35 seconds. However, for a client on heparin therapy, the target PTT is typically 1.5 to 2.5 times the normal range, which would be approximately 60 to 80 seconds. Since the client’s PTT is only 25 seconds, it indicates that the blood is clotting too quickly, and the heparin dose is insufficient.
Choice B reason: Decreasing the heparin rate would further reduce the anticoagulant effect, which is not advisable given the current PTT of 25 seconds. Lowering the heparin rate could increase the risk of thrombus formation and worsen the deep vein thrombosis (DVT) condition.
Choice C reason: Stopping heparin and starting warfarin is not an immediate solution. Warfarin takes several days to achieve its full anticoagulant effect, and during this transition period, the client would be at risk of clot formation. Heparin provides immediate anticoagulation, which is crucial in the acute management of DVT.
Choice D reason: Increasing the heparin rate is the correct action. The current PTT of 25 seconds is below the therapeutic range for a client on heparin therapy. Increasing the heparin rate will help achieve the desired anticoagulant effect, prolonging the PTT to the target range of 60 to 80 seconds.
Correct Answer is ["B","C","E"]
Explanation
Choice A: Lean on your back with your knees bent.
Reason: This instruction is incorrect. Pursed lip breathing is typically performed in a seated position with the neck and shoulders relaxed. Lying on your back with knees bent is not a recommended position for this breathing technique.
Choice B: Use your abdominal muscles to squeeze air out of your lungs.
Reason: This instruction is correct. Using the abdominal muscles helps to expel air more effectively from the lungs, which is a key component of pursed lip breathing. This technique helps to improve ventilation and reduce the work of breathing.
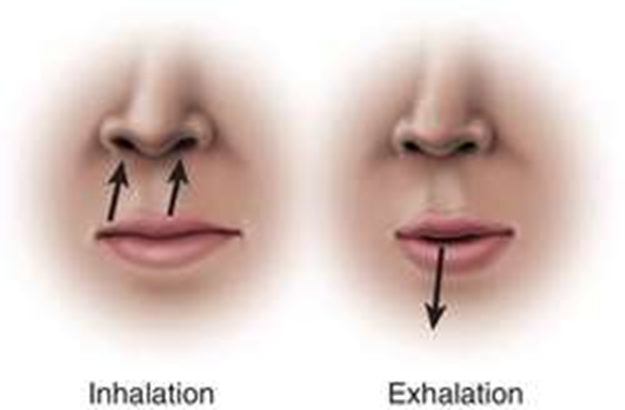
Choice C: Breathe out slowly without puffing your cheeks.
Reason: This instruction is correct. Breathing out slowly through pursed lips without puffing the cheeks helps to keep the airways open longer, allowing more air to be expelled from the lungs. This technique is particularly beneficial for individuals with chronic obstructive pulmonary disease (COPD) or other respiratory conditions.
Choice D: Focus on inhaling and holding your breath as long as you can.
Reason: This instruction is incorrect. The focus of pursed lip breathing is on controlled exhalation rather than holding the breath. Inhaling should be done slowly through the nose, and exhaling should be prolonged through pursed lips.
Choice E: Exhale at least twice the amount of time it took to breathe in.
Reason: This instruction is correct. The exhalation phase should be longer than the inhalation phase, typically taking at least twice as long. This helps to improve the efficiency of breathing and reduce shortness of breath.
Choice F: Open your mouth and breathe deeply.
Reason: This instruction is incorrect. Pursed lip breathing involves breathing in through the nose and exhaling through pursed lips. Opening the mouth and breathing deeply is not part of this technique.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
