An oil retention enema is prescribed for a hospitalized client. The practical nurse (PN) should administer the enema solution at which temperature?
The solution temperature should be determined by the client’s comfort level
The temperature of the enema is unrelated to the enema’s effectiveness
The solution should approximate the client’s body temperature (98°F or 36°C).
The temperature should be higher (110°F or 43°C) than the client’s body temperature
The Correct Answer is C
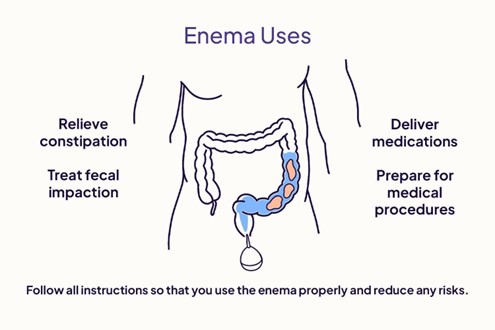
- An oil retention enema is used to soften the stool and lubricate the rectum, making it easier to pass the stool. It is usually oil-based and contains 90-120 ml of solution³.
- The temperature of the enema solution affects the effectiveness and comfort of the procedure. If the solution is too hot or cold, it can cause pain, cramps, or damage to the rectal tissue³. If the solution is too warm, it can also stimulate peristalsis and cause the client to expel the enema before it has time to work⁴.
- The ideal temperature for an enema solution is close to the client’s body temperature, which is around 98°F or 36°C. This temperature ensures that the solution is comfortable and does not cause adverse reactions³⁴.
Option A is incorrect because the client’s comfort level may not reflect the optimal temperature for the
enema.
Option B is incorrect because the temperature of the enema does affect its effectiveness and safety. Option D is incorrect because the temperature is too high and can cause harm to the client.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: Encouraging community members to practice fire drills is an activity that is a part of the prevention/mitigation phase of the disaster management cycle because it can reduce the risk of injury or death from fire by increasing the awareness and preparedness of the community.
Choice B reason: Identifying community members who have disabilities is an activity that is a part of the prevention/mitigation phase of the disaster management cycle because it can reduce the vulnerability of these individuals by ensuring that they have access to appropriate resources and assistance in case of a disaster.
Choice C reason: Providing first aid to community members affected by a tornado is not an activity that is a part of the prevention/mitigation phase of the disaster management cycle, but rather the response phase, which involves delivering immediate and short-term assistance to save lives and meet basic needs during and after a disaster.
Choice D reason: Assisting community members in developing a disaster plan is not an activity that is a part of the prevention/mitigation phase of the disaster management cycle, but rather the preparedness phase, which involves enhancing the readiness and capabilities of individuals, organizations, and communities to respond to and recover from a disaster.
Correct Answer is ["A","C","E"]
Explanation
Choice A reason: Asking how they are managing at home is an appropriate action by the nurse because it shows interest and respect for the client's situation, needs, and preferences.
Choice B reason: Going automatically into the client's bedroom is not an appropriate action by the nurse because it violates the client's privacy and autonomy. The nurse should ask for permission before entering any room in the client's homE.
Choice C reason: Arranging mutual future visits is an appropriate action by the nurse because it demonstrates collaboration and continuity of care with the client.
Choice D reason: Thanking the client for arranging a home visit is not an appropriate action by the nurse because it implies that the nurse is doing a favor for the client, rather than providing professional servicE.
Choice E reason: Sitting down and discussing with the client and family members is an appropriate action by the nurse because it facilitates communication, rapport, and education with the client and their support system.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
