A patient with Parkinson's disease asks the nurse why anticholinergics are used in the treatment. Which response by the nurse is most accurate?
"These drugs inhibit the action of acetylcholine
"These drugs help you urinate."
"These drugs will decrease your eye pressure."
"These drugs will assist in lowering your heart rate."
The Correct Answer is A
A. "These drugs inhibit the action of acetylcholine":
This response is accurate. Anticholinergic medications work by blocking the action of acetylcholine, a neurotransmitter involved in various functions in the body, including muscle control. In Parkinson's disease, there is an imbalance between dopamine and acetylcholine, leading to motor symptoms such as tremors and rigidity. By inhibiting the action of acetylcholine, anticholinergic drugs help rebalance neurotransmitter activity and alleviate some of the motor symptoms associated with Parkinson's disease.
B. "These drugs help you urinate":
This statement is not directly related to the use of anticholinergic medications in Parkinson's disease. While some anticholinergic drugs can indeed relax the smooth muscle of the bladder and improve urinary symptoms, this is not the primary indication for their use in Parkinson's disease.
C. "These drugs will decrease your eye pressure":
While anticholinergic medications can be used to dilate the pupils and decrease intraocular pressure, this is not typically the reason for their use in Parkinson's disease. While some anticholinergic medications may have ocular effects, they are primarily used to address motor symptoms associated with Parkinson's disease.
D. "These drugs will assist in lowering your heart rate":
While some anticholinergic medications may have effects on heart rate by blocking parasympathetic nervous system activity, this is not the primary indication for their use in Parkinson's disease. The focus of anticholinergic therapy in Parkinson's disease is primarily on addressing motor symptoms rather than cardiovascular effects.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Pupil response:
Pupil response refers to the reaction of the pupils to light stimulus. The pupils should normally constrict when exposed to bright light and dilate in dim light. Changes in pupil size or reactivity can indicate alterations in neurological function. For example, unequal or non-reactive pupils (anisocoria or fixed pupils) can be indicative of dysfunction in the cranial nerves or brainstem. However, while pupil response is an important aspect of neurological assessment, it may not always be the earliest indicator of cerebral status changes.
B. Deep tendon reflexes:
Deep tendon reflexes are involuntary muscle contractions in response to stretching of a muscle tendon. These reflexes are assessed by tapping the tendon with a reflex hammer, eliciting a rapid and brief muscle contraction. Changes in deep tendon reflexes can provide information about the integrity of the peripheral nervous system and spinal cord. However, alterations in deep tendon reflexes may occur secondary to changes in cerebral function and are typically assessed along with other neurological signs.
C. Muscle strength:
Muscle strength refers to the force generated by muscles during voluntary movement. It is typically assessed by asking the client to perform specific movements against resistance or by testing the strength of individual muscle groups using standardized scales (e.g., Medical Research Council scale). Changes in muscle strength can occur due to neurological or musculoskeletal conditions. While weakness or paralysis can result from lesions affecting the upper motor neurons (e.g., strokes or spinal cord injuries), alterations in muscle strength may not always be the earliest indicator of cerebral status changes.
D. Level of consciousness:
The level of consciousness refers to the degree of awareness and alertness exhibited by the client. It is assessed by evaluating the client's responsiveness, orientation, and ability to follow commands. Changes in the level of consciousness, such as confusion, lethargy, stupor, or coma, can indicate alterations in cerebral function and are often the earliest indicators of neurological dysfunction. Assessing the level of consciousness is a critical component of neurological examination and helps guide further assessment and management of clients with suspected brain tumors or other neurological conditions.
Correct Answer is B
Explanation
A. Decreased pedal pulses:
Decreased pedal pulses are not typically associated with increased intracranial pressure. Instead, they may indicate peripheral vascular disease or reduced perfusion to the lower extremities. Monitoring peripheral pulses is important for assessing circulation but is not directly related to intracranial pressure changes.
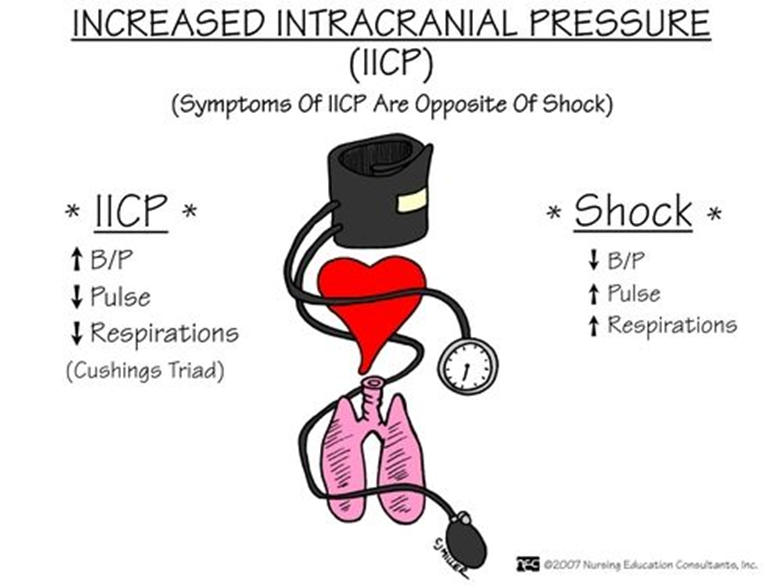
B. Hypertension:
Hypertension can be a manifestation of increased intracranial pressure. The body may respond to elevated intracranial pressure by increasing blood pressure to maintain cerebral perfusion pressure. However, hypertension alone is not specific to increased ICP and can have various causes.
C. Peripheral edema:
Peripheral edema is not a typical manifestation of increased intracranial pressure. It may occur in conditions such as heart failure or renal dysfunction but is not directly related to intracranial pressure changes following a craniotomy.
D. Diarrhea:
Diarrhea is not a common manifestation of increased intracranial pressure. Increased ICP is more likely to manifest with symptoms such as headache, nausea, vomiting, altered level of consciousness, and focal neurological deficits.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
