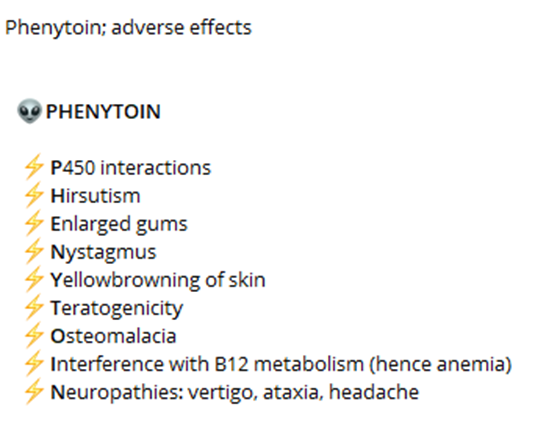
A nurse is reinforcing teaching a client who has a new prescription for phenytoin. The nurse should instruct the client to monitor and report which of the following adverse effects of this medication?
Diarrhea
Wrist pain
Skin rash
Metallic taste
The Correct Answer is C
A. Diarrhea:
Diarrhea is not a common side effect of phenytoin. While gastrointestinal disturbances such as nausea, vomiting, and constipation may occur, diarrhea is less common. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
B. Wrist pain:
Wrist pain is not a common side effect of phenytoin. Side effects related to musculoskeletal issues such as joint pain, muscle weakness, or muscle twitching can occur, but wrist pain specifically is not commonly associated with phenytoin use. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
C. Skin rash:
Skin rash is a potential adverse effect of phenytoin that should be monitored and reported. Phenytoin can cause various skin reactions, including a mild rash or more severe reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis. Therefore, the nurse should instruct the client to promptly report any signs of skin rash or other skin changes.
D. Metallic taste:
Metallic taste is a common side effect of phenytoin. While it is not usually a serious adverse effect, it can be bothersome for some individuals. Therefore, the nurse should instruct the client to monitor for this side effect and report it if it occurs persistently or becomes bothersome.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
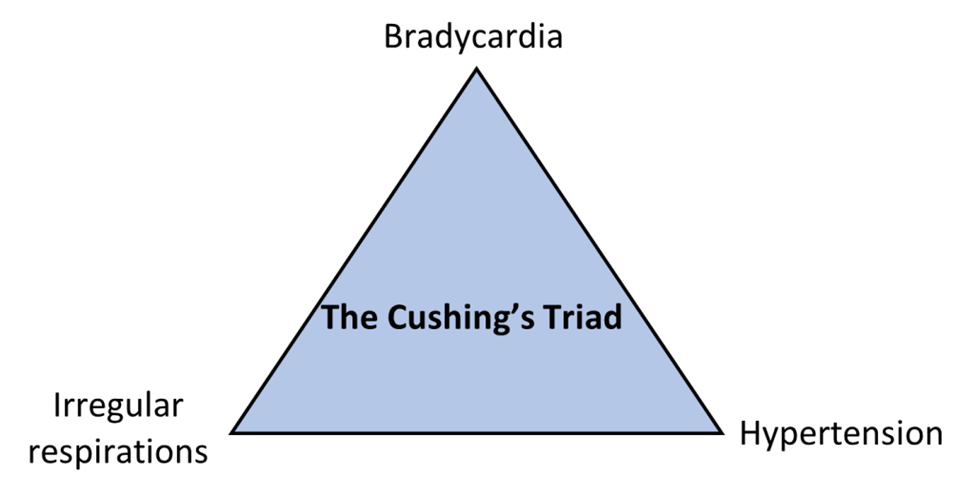
Correct Answer is A
Explanation
A. Bradycardia, hypertension, and widening pulse pressure
This combination of symptoms is characteristic of Cushing's triad. Bradycardia (slow heart rate), hypertension (elevated blood pressure), and widening pulse pressure (difference between systolic and diastolic blood pressure) are indicative of increased ICP, specifically resulting in the compression of brain structures that regulate vital functions.
B. Widening pulse pressure, headache, and seizure
While headache and seizure may occur in patients with increased ICP, widening pulse pressure alone is not sufficient to meet the criteria of Cushing's triad. The presence of bradycardia and hypertension, along with widening pulse pressure, is more indicative of Cushing's triad.
C. Hypertension, tachycardia, and headache
Hypertension and headache may occur in patients with increased ICP, but the absence of bradycardia and widening pulse pressure makes this option less characteristic of Cushing's triad.
D. Hypotension, tachycardia, and narrowing pulse pressure
Hypotension (low blood pressure) and narrowing pulse pressure are not typically associated with Cushing's triad. Tachycardia (rapid heart rate) may occur in response to increased ICP, but it is usually accompanied by bradycardia rather than hypotension.
Correct Answer is A
Explanation
A. "It is too early to tell. When the spinal shock subsides, we will know more."
This response is appropriate. Spinal shock can initially obscure the extent of neurological injury, and it may take time for the full extent of the injury to become apparent. By acknowledging this and suggesting that more information will be available once spinal shock subsides, the nurse provides a realistic perspective without prematurely predicting the outcome.
B. "You should talk to your physician about things of that nature."
This response may come across as dismissive or evasive. While it is true that the physician ultimately determines the patient's prognosis, the family may be seeking reassurance and guidance from the nurse as well.
C. "No. Significant recovery of function should occur in a few days."
This response is overly optimistic and potentially misleading. While some improvement may occur in the days following a spinal cord injury, significant recovery of function within a few days is unlikely, especially in cases of flaccid paralysis of all extremities.
D. "Yes. In all likelihood, the paralysis is probably permanent."
This response is overly pessimistic and lacks sensitivity. It may unnecessarily distress the family and extinguish hope for the patient's recovery.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
