A nurse is teaching a client diagnosed with gastroesophageal reflux disease (GERD) about managing their Illness. Which of the following recommendations should the nurse include in the teaching?
Limit fluid intake not related to meals.
Avoid eating within 3 hr of bedtime
Chew on mint leaves to relieve indigestion.
Season foods with black pepper.
The Correct Answer is B
A. Limit fluid intake not related to meals:
While staying hydrated is important, it's generally recommended to limit fluid intake not related to meals to avoid overfilling the stomach and putting excess pressure on the lower esophageal sphincter (LES). However, this is not as specific to GERD management as the option B.
B. Avoid eating within 3 hours of bedtime:
This is a key recommendation for managing GERD. Eating close to bedtime increases the likelihood of stomach contents refluxing into the esophagus when lying down. Waiting at least 3 hours after eating before lying down can help prevent symptoms.
C. Chew on mint leaves to relieve indigestion:
Mint, including mint leaves, can relax the LES, potentially worsening GERD symptoms. It is not recommended for managing GERD.
D. Season foods with black pepper:
While black pepper itself is not a common trigger for GERD, highly spicy or peppery foods can sometimes exacerbate symptoms in individuals with GERD. It's advisable to pay attention to personal triggers and adjust the diet accordingly.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
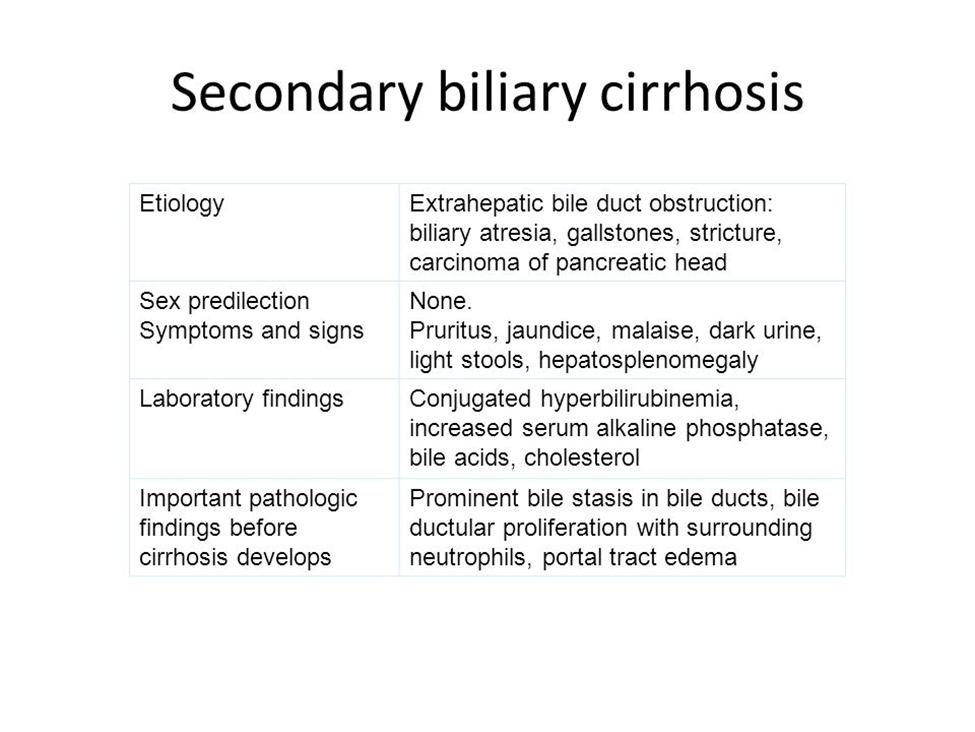
A. Obstruction of the bile duct:
Biliary cirrhosis can result from chronic obstruction of the bile ducts, leading to damage to the liver tissue. This obstruction can be due to various causes, such as gallstones or strictures.
B. Hepatotoxic medications:
While certain medications can contribute to liver damage, biliary cirrhosis specifically refers to conditions affecting the bile ducts. Hepatotoxic medications may contribute to cirrhosis but not necessarily biliary cirrhosis.
C. Hepatitis C:
Hepatitis C is a viral infection that primarily affects the liver. While chronic hepatitis C infection can lead to cirrhosis, it is not synonymous with biliary cirrhosis.
D. Excessive alcohol consumption:
Excessive alcohol consumption is a common cause of cirrhosis, but biliary cirrhosis specifically refers to cirrhosis resulting from chronic obstruction of the bile ducts.
Correct Answer is A
Explanation
A. "Eat four small meals each day":
Smaller, more frequent meals reduce gastric distension and lower gastric pressure, which decreases reflux of stomach contents into the esophagus. Large meals increase intra-abdominal pressure and worsen GERD symptoms.
B. "Sleep on your left side":
Sleeping on the left side may reduce symptoms of GERD for some individuals. This position can keep the stomach below the esophagus, minimizing reflux. However, individual preferences and comfort should be considered.
C. "Wait to go to bed for 1 hour after eating":
This instruction helps reduce the risk of reflux while lying down. Waiting after eating allows gravity to aid in digestion and reduces the likelihood of stomach contents backing up into the esophagus during sleep.
D. "Drink milk to soothe your stomach":
While milk might provide temporary relief for some people by neutralizing stomach acid, it can stimulate acid production, potentially exacerbating GERD symptoms in the long run. Therefore, it's not a recommended solution for managing GERD.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
