A nurse is reinforcing teaching about diagnostic tests with the parents of a child who has suspected cystic fibrosis. Which of the following diagnostic tests should the nurse include as the most definitive when diagnosing cystic fibrosis?
Pulmonary function test
Sweat chloride test
Stool fat content analysis
Sputum culture
The Correct Answer is B
A. Pulmonary function test:
Pulmonary function tests (PFTs) assess lung function by measuring airflow, lung volume, and gas exchange. While PFTs can provide valuable information about respiratory function, they are not specific to cystic fibrosis and may show abnormalities consistent with various respiratory conditions. However, PFTs are often performed in individuals with cystic fibrosis to monitor lung function over time and assess response to treatment. They are not considered the most definitive test for diagnosing cystic fibrosis.
B. Sweat chloride test:
This option is correct. The sweat chloride test is considered the most definitive diagnostic test for cystic fibrosis. It measures the concentration of chloride in sweat, which is typically elevated in individuals with cystic fibrosis due to defective chloride transport in sweat glands. A sweat chloride concentration above a certain threshold (usually ≥60 mmol/L) is diagnostic of cystic fibrosis, particularly when confirmed with repeat testing.
C. Stool fat content analysis:
Stool fat content analysis evaluates fat absorption and fecal fat excretion, which may be impaired in individuals with cystic fibrosis due to pancreatic insufficiency. However, while stool fat content analysis can provide supportive evidence of malabsorption in cystic fibrosis, it is not considered the most definitive test for diagnosing the condition. Stool fat content analysis is often used in conjunction with other diagnostic tests to assess pancreatic function and nutritional status in individuals with cystic fibrosis.
D. Sputum culture:
Sputum culture involves culturing respiratory secretions to identify bacterial pathogens, which can be useful for diagnosing respiratory infections in individuals with cystic fibrosis. However, sputum culture is not specific to cystic fibrosis and may show similar findings in other respiratory conditions. While respiratory cultures are important for guiding treatment in cystic fibrosis, they are not considered the most definitive test for diagnosing the condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
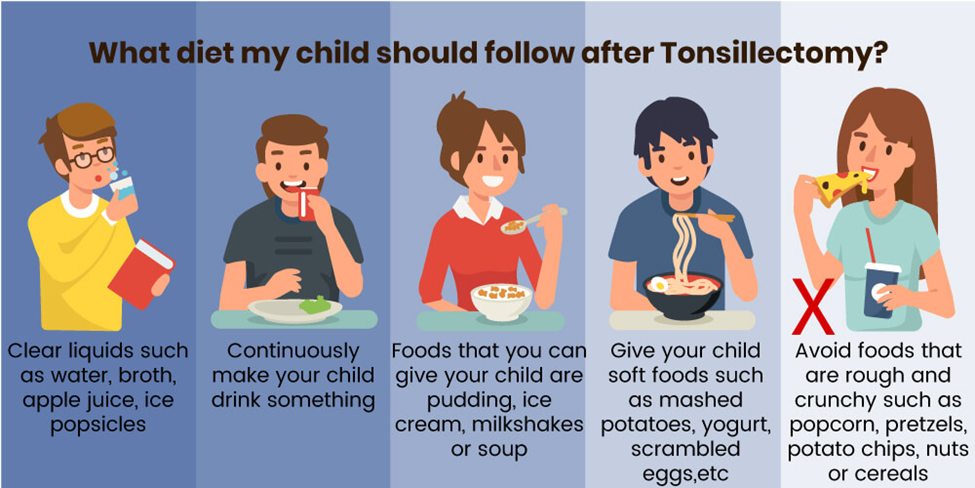
Correct Answer is ["B","D"]
Explanation
A. Cranberry juice
Cranberry juice may be too acidic and could irritate the surgical site. It's best to avoid acidic beverages immediately following a tonsillectomy.
B. Ice-cream
This option is suitable. Ice-cream is cold and soothing, and it can help numb the throat, providing relief from discomfort after a tonsillectomy. However, it's essential to ensure that the ice-cream is not too cold to avoid causing discomfort.
C. Hot tea
Hot tea is not recommended immediately following a tonsillectomy. Hot liquids can irritate the surgical site and may cause discomfort. It's best to avoid hot beverages until the throat has had time to heal.
D. Italian ice
Italian ice is a frozen dessert similar to a slushy, and it can be a suitable option after a tonsillectomy. Like ice-cream, Italian ice is cold and can help numb the throat, providing relief from discomfort.
Correct Answer is D
Explanation
A. Place the infant in prone position.
This option is incorrect. Placing the infant in the prone position (lying on the stomach) could put pressure on the spinal lesion, potentially causing discomfort or complications. It's important to minimize pressure on the affected area in infants with spina bifida.
B. Cover the infant's lesion with a dry cloth.
This option is incorrect. While keeping the lesion clean and dry is important for preventing infection, simply covering it with a dry cloth may not provide adequate protection. Proper wound care techniques, such as using sterile dressings and cleaning the area with prescribed solutions, are typically necessary to prevent infection and promote healing.
C. Feed the infant through an NG tube.
This option is incorrect. While infants with severe forms of spina bifida may have difficulty feeding due to associated complications, such as difficulty swallowing or weak sucking reflexes, feeding through a nasogastric (NG) tube is not a standard intervention for spina bifida itself. Feeding methods would depend on the specific needs and abilities of the infant, and may involve breastfeeding, bottle-feeding, or other methods under the guidance of healthcare professionals.
D. Diapering over a low defect will keep the infant free from infection.
This option is correct. Diapering over a low defect (the opening in the spine caused by spina bifida) helps to keep the area clean and reduce the risk of infection. By properly covering the defect with a diaper, exposure to urine and feces, which can increase the risk of infection, is minimized. Additionally, regular diaper changes and proper hygiene practices are essential for preventing complications in infants with spina bifida.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
