A nurse is caring for a child who has Kawasaki disease. Which of the following systems should the nurse monitor in response to this diagnosis?
Gastrointestinal
Respiratory
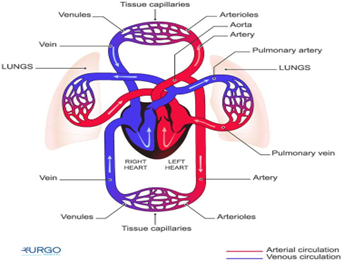
Cardiovascular
Integumentary
The Correct Answer is C
A. Gastrointestinal:
Kawasaki disease primarily affects blood vessels, and the gastrointestinal system is not the main target of this condition. While gastrointestinal symptoms can occur as part of the overall inflammatory response, such as abdominal pain, vomiting, or diarrhea, they are not the primary focus of concern in Kawasaki disease. The most critical system to monitor in Kawasaki disease is the cardiovascular system, specifically the coronary arteries.
B. Respiratory:
The respiratory system is not the primary system affected by Kawasaki disease. While respiratory symptoms can occur as part of the overall inflammatory response and fever associated with the disease, such as coughing or runny nose, they are not the main concern in Kawasaki disease. The primary system to monitor in this condition is the cardiovascular system, especially the coronary arteries.
C. Cardiovascular:
This is the correct answer. Kawasaki disease is primarily a vasculitis (inflammation of blood vessels) that affects various blood vessels, including the coronary arteries. The inflammation of the coronary arteries can lead to coronary artery aneurysms and other cardiac complications. Monitoring the cardiovascular system is essential to detect any signs of coronary artery involvement and ensure timely intervention to prevent potential long-term cardiac problems.
D. Integumentary:
The integumentary system (skin) is not the primary focus of Kawasaki disease. While some skin changes can occur during the acute phase of the disease, such as a rash or peeling skin on the hands and feet, these are not the primary concerns. Monitoring the cardiovascular system is critical in Kawasaki disease due to the risk of coronary artery inflammation and potential complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Cystic fibrosis (CF) is a genetic disorder that affects the production and function of certain glands, particularly those that produce mucus and sweat. One of the key aspects of CF management is addressing the pancreatic insufficiency that occurs in many individuals with CF. Due to the impairment of the pancreas, children with CF may have difficulty digesting food properly, especially fats. This can lead to malabsorption of nutrients, poor weight gain, and other nutritional deficiencies.
Pancreatic enzyme replacement therapy is a crucial part of CF management. Pancreatic enzymes are prescribed to help the child digest and absorb essential nutrients, especially fats. The enzymes are typically given with each meal and snack to aid in the breakdown and absorption of nutrients.
The other options are not correct:
A. "We will restrict the amount of salt in our child's food."
Sodium restriction is generally not a focus in CF management unless there are specific indications for it. CF patients may have increased salt losses in sweat, but dietary sodium restriction is not a primary aspect of their care.
B. "I will limit my child's fluid intake."
Fluid intake is important for children with CF to maintain hydration and prevent dehydration. There is no specific need to limit fluid intake unless there are individualized medical reasons for doing so.
C. "I will prepare low-fat meals with limited protein for my child."
Children with CF often require a high-calorie, high-protein diet to maintain adequate nutrition and growth. Restricting fat and protein intake is not typically recommended, as these nutrients are essential for a child's development and well-being. Instead, pancreatic enzymes are used to aid in the digestion and absorption of fats and other nutrients.
Correct Answer is A
Explanation
The nurse should expect to find irritability in an infant who is dehydrated. Dehydration in infants can lead to changes in behavior and irritability due to the imbalance in fluid and electrolytes. Other common signs of dehydration in infants may include:
Poor skin turgor (skin tenting)
Sunken fontanelles (soft spots on the baby's head)
Dry mucous membranes (dry mouth and tongue)
Decreased urine output or concentrated urine
Rapid heart rate (tachycardia)
Increased respiratory rate
Sunken eyes
Decreased tears when crying
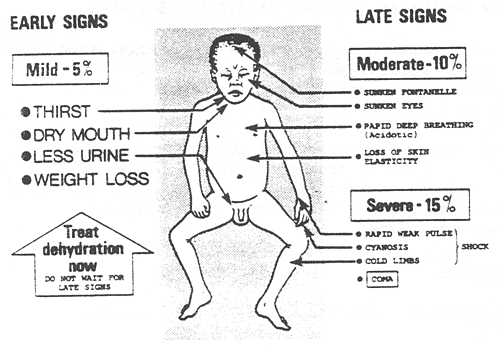
B. Tetany is a condition characterized by involuntary muscle contractions and is more commonly associated with hypocalcemia (low calcium levels) rather than dehydration.
C. A slow, bounding pulse is not typically associated with dehydration. Dehydration often leads to a rapid heart rate (tachycardia) as the body attempts to compensate for the loss of fluid.
D. Decreased temperature is not a typical finding in dehydration. Dehydration can lead to fever in some cases due to an underlying infection, but it does not cause a decrease in body temperature on its own.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
