A nurse is planning care for a client who has neurogenic shock following a spinal cord injury. Which of the following provider prescriptions should the nurse anticipate? (Select all that apply.)
(Select All that Apply.)
Metoprolol
Lactated Ringers intravenous fluid
Furosemide
Dopamine
Epinephrine
Correct Answer : B,D,E
Choice A Reason:
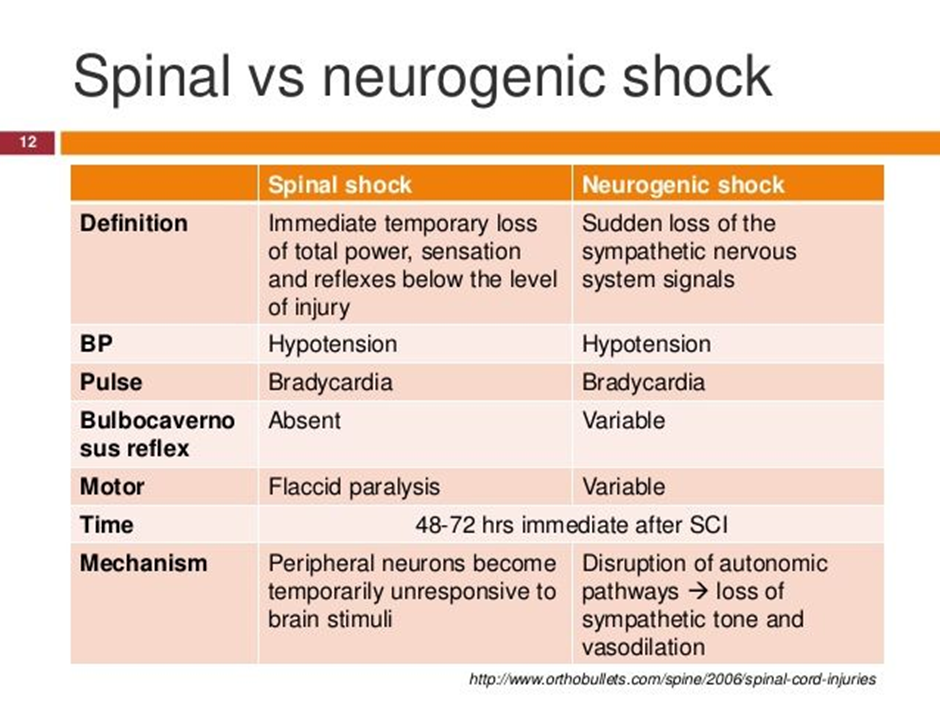
Metoprolol is incorrect. Metoprolol is a beta-blocker medication commonly used to treat conditions such as hypertension, angina, and heart failure. However, in the context of neurogenic shock following a spinal cord injury, the use of beta-blockers such as metoprolol is generally contraindicated. Beta-blockers antagonize the effects of sympathetic activation, leading to a reduction in heart rate and myocardial contractility, which can exacerbate hypotension and bradycardia, the hallmarks of neurogenic shock. Therefore, the nurse would not anticipate a prescription for metoprolol in the management of neurogenic shock.
Choice B Reason:
Lactated Ringers intravenous fluid is correct. Fluid resuscitation with isotonic crystalloid solutions such as lactated Ringers is essential to restore intravascular volume and improve perfusion.
Choice C Reason:
Furosemide is incorrect. Furosemide is a loop diuretic medication commonly used to treat conditions such as heart failure, edema, and hypertension by promoting diuresis and reducing fluid volume. However, in the context of neurogenic shock, the use of diuretics such as furosemide is generally not indicated unless there is concurrent volume overload. Neurogenic shock is characterized by hypotension due to vasodilation and decreased systemic vascular resistance, often leading to relative hypovolemia rather than volume overload. Therefore, administering furosemide could further decrease intravascular volume, exacerbating hypotension and compromising perfusion. As a result, the nurse would not anticipate a prescription for furosemide in the management of neurogenic shock.:
Choice D Reason:
Dopamine is correct. Dopamine is a vasopressor medication that acts to increase vascular tone and blood pressure by stimulating alpha-adrenergic receptors. It is commonly used in the management of neurogenic shock to augment blood pressure.
Choice E Reason:
Epinephrine is correct. Epinephrine is a potent vasopressor that acts on both alpha and beta-adrenergic receptors, leading to vasoconstriction and increased cardiac output. It is used in the treatment of refractory hypotension in neurogenic shock.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Vasogenic cerebral edema is appropriate response. Vasogenic cerebral edema occurs due to disruption of the blood-brain barrier (BBB), leading to leakage of fluid and proteins from the blood vessels into the brain parenchyma. This type of cerebral edema is commonly associated with conditions such as brain tumors, abscesses, and ischemic stroke.
Choice B Reason:
Osmotic cerebral edema is inappropriate response. Osmotic cerebral edema occurs when there is an imbalance of osmotic forces across the blood-brain barrier, leading to the movement of water into the brain cells. This type of cerebral edema can result from conditions such as hyponatremia or the administration of hypertonic solutions.
Choice C Reason:
Cellular cerebral edema is inappropriate response. Cellular cerebral edema involves the swelling of brain cells (neurons and glial cells) due to various insults, such as ischemia, hypoxia, or metabolic disturbances. This type of cerebral edema can occur in conditions such as ischemic stroke or traumatic brain injury.
Choice D Reason:
Interstitial cerebral edema is incorrect response. Interstitial cerebral edema involves the accumulation of fluid within the interstitial spaces of the brain tissue. This type of cerebral edema can occur in conditions such as hydrocephalus, where there is obstruction of cerebrospinal fluid (CSF) flow.
Correct Answer is D
Explanation
"The nerves just go to sleep when I lie down because no message gets from my brain to the spinal cord." is incorrect because it does not accurately describe the mechanism of peripheral neuropathy. Peripheral neuropathy in diabetes is not simply the nerves "going to sleep" due to lack of communication between the brain and spinal cord.
Choice B Reason:
"The nerve damage may occur for unknown reasons in any individual" is incorrect because while the exact cause of peripheral neuropathy may not always be known, in the context of diabetes mellitus, the link between elevated blood sugar levels and nerve damage is well-established.
Choice C Reason:
"The older I get, there is less blood flowing to my feet. “is incorrect because while decreased blood flow (ischemia) can contribute to peripheral neuropathy in some cases, the primary mechanism in diabetic neuropathy is nerve damage due to hyperglycemia rather than reduced blood flow.
Choice D Reason:
"The elevated blood sugar from my diabetes can cause underlying nerve damage." Peripheral neuropathy is a common complication of diabetes mellitus, particularly when the condition is uncontrolled. Elevated blood sugar levels over time can lead to damage to the nerves, especially those in the feet and legs. This damage can result in symptoms such as numbness, tingling, burning sensations, or pain in the affected areas.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
