A nurse is collecting data from a client who has gastroesophageal reflux disease (GERD) and reports having heartburn every night. Which of the following actions should the nurse identify as a contributing factor to the client’s heartburn?
Drinking orange juice regularly
Eating dinner early in the evening
Consuming low-fat meats
Sleeping on a large wedge-style pillow
The Correct Answer is A
Choice A: Drinking orange juice regularly. This is a contributing factor to the client’s heartburn because orange juice is acidic and can irritate the esophageal mucosa and lower esophageal sphincter, causing reflux of gastric contents into the esophagus.
Choice B: Eating dinner early in the evening. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should avoid eating within 3 hours of bedtime to allow for gastric emptying and reduce the risk of reflux.
Choice C: Consuming low-fat meats. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should avoid high-fat foods, which can delay gastric emptying and increase intra-abdominal pressure, leading to reflux.
Choice D: Sleeping on a large wedge-style pillow. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should elevate the head of their bed or use a wedge pillow to create an incline that prevents gastric contents from flowing back into the esophagus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: Dysphagia. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Dysphagia is difficulty swallowing, which can be caused by disorders of the esophagus, throat, or nervous system. It is not related to hyperparathyroidism or calcium and phosphorus levels.
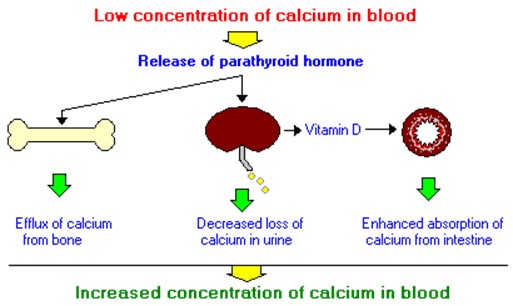
Choice B: Pathologic fractures. This is a complication that the nurse should monitor the client for who has hyperparathyroidism, which is a condition that occurs when the parathyroid glands produce too much parathyroid hormone (PTH). PTH regulates calcium and phosphorus levels in the blood and bones. Hyperparathyroidism can cause hypercalcemia, which is a high level of calcium in the blood, and hypophosphatemia, which is a low level of phosphorus in the blood. These imbalances can lead to bone resorption, which is the breakdown of bone tissue and release of calcium into the blood. Bone resorption can weaken the bones and increase the risk of pathologic fractures, which are fractures that occur due to disease or injury to the bone.
Choice C: Fluid retention. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Fluid retention is excess fluid accumulation in the body, which can be caused by disorders of the heart, kidney, liver, or lymphatic system. It is not related to hyperparathyroidism or calcium and phosphorus levels.
Choice D: Impaired skin integrity. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Impaired skin integrity is damage or loss of skin tissue, which can be caused by trauma, infection, inflammation, or pressure. It is not related to hyperparathyroidism or calcium and phosphorus levels.
Correct Answer is ["A","C","E"]
Explanation
Choice A: Purple striations. These are also known as striae, and they are caused by the thinning and weakening of the skin and underlying connective tissue due to cortisol. They appear as purple or red lines on the abdomen, thighs, breasts, or arms.
Choice C: Buffalo hump. This is a term used to describe the accumulation of fat on the upper back and neck due to cortisol. It gives the appearance of a hump or a rounded shape.
Choice E: Moon face. This is a term used to describe the rounding and fullness of the face due to cortisol. It gives the
appearance of a moon-like shape.
Choice B: Tremors. These are not a clinical manifestation of Cushing’s syndrome, but rather a sign of hyperthyroidism, which is a condition caused by excess thyroid hormone production or exposure. Thyroid hormone affects the nervous system and causes increased muscle activity and tremors.
Choice D: Obese extremities. These are not a clinical manifestation of Cushing’s syndrome, but rather a sign of hypothyroidism, which is a condition caused by low thyroid hormone production or exposure. Thyroid hormone affects the metabolism of carbohydrates, proteins, and fats, and causes decreased energy expenditure and weight gain.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
