The nurse is caring for a client who has a bowel obstruction and a new prescription for the insertion of a nasogastric tube. Which of the following interventions should the nurse take when inserting the nasogastric tube?
Measure the tube for insertion from the tip of the nose to the umbilicus.
Place the client in a supine position.
Withdraw the tube if the client gags during insertion.
Instruct the client to place his chin to his chest and swallow.
The Correct Answer is D
Choice A: Measure the tube for insertion from the tip of the nose to the umbilicus. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should measure the tube for insertion from the tip of the nose to the earlobe and then to the xiphoid process, which is a more accurate way of estimating the length of the tube needed to reach the stomach.
Choice B: Place the client in a supine position. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should place the client in a high-Fowler’s position, which is a position with the head of the bed elevated to 90 degrees. This position can prevent aspiration, promote breathing, and allow gravity to assist with the insertion of the tube.
Choice C: Withdraw the tube if the client gags during insertion. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should not withdraw the tube if the client gags during insertion, as this can cause trauma to the nasal or pharyngeal mucosa and increase discomfort. The nurse should pause and allow the client to rest and breathe until gagging subsides, then resume insertion. The nurse should also provide reassurance and encouragement to the client throughout the procedure.
Choice D: Instruct the client to place his chin to his chest and swallow. This is an intervention that the nurse should take when inserting a nasogastric tube, which is a flexible tube that is inserted through the nose and into the stomach. The nurse should instruct the client to place his chin to his chest and swallow as the tube passes through the pharynx and into the esophagus. This can facilitate the insertion of the tube and prevent it from entering the trachea or causing injury to the nasal or pharyngeal mucosa.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
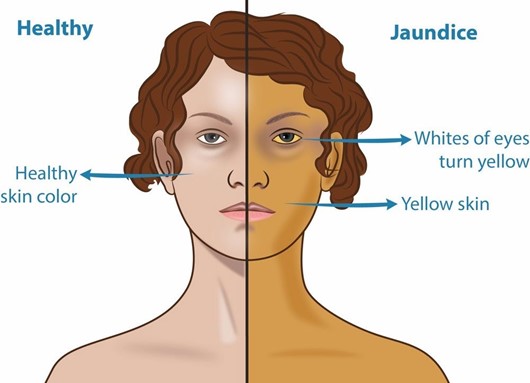
Choice A: Peri-umbilical area. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The peri-umbilical area is the area around the navel, which is part of the skin. The skin can show jaundice, but it may be difficult to detect in clients with dark skin tones.
Choice B: Nail beds. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The nail beds are part of the skin that can show jaundice, but they may also be affected by other factors such as anemia, cyanosis, or nail polish.
Choice C: Webbed areas of the fingers. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The webbed areas of the fingers are part of the skin that can show jaundice, but they may also be influenced by other factors such as temperature, circulation, or pressure.
Choice D: Hard palate. This is an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis, which is an inflammation of the gallbladder. Jaundice is a yellowish discoloration of the skin and mucous membranes due to elevated bilirubin levels in the blood. Bilirubin is a pigment that is produced from the breakdown of red blood cells and is normally excreted in bile. If the gallbladder or bile ducts are inflamed or obstructed, bile cannot flow into the duodenum and bilirubin accumulates in the blood and tissues. The hard palate is a part of the oral mucosa that can show jaundice, especially in clients with dark skin tones.
Correct Answer is A
Explanation
Choice A: Potassium 2.5 mEq/L. This is the priority data collection finding that the nurse should identify according to the ABCDE principle, which prioritizes interventions based on airway, breathing, circulation, disability, and exposure. The nurse should identify potassium 2.5 mEq/L as the priority because it indicates hypokalemia, which is a low level of potassium in the blood. Potassium is an electrolyte that regulates the electrical activity of the heart and muscles. Hypokalemia can cause cardiac arrhythmias, muscle weakness, and paralysis, which can be life-threatening.
Choice B: Blood glucose 150 mg/dL. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Blood glucose 150 mg/dL indicates hyperglycemia, which is a high level of glucose in the blood. Hyperglycemia can be caused by dehydration, stress, infection, or medication side effects.
Hyperglycemia can cause symptoms such as polyuria, polydipsia, polyphagia, and fatigue. It can also lead to complications such as diabetic ketoacidosis or hyperosmolar hyperglycemic state, which are serious but not as urgent as hypokalemia.
Choice C: Urine specific gravity 1.035. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Urine specific gravity 1.035 indicates concentrated urine, which can be caused by dehydration or fluid loss. Dehydration can result from vomiting and diarrhea, which are common symptoms of acute gastroenteritis. Dehydration can cause symptoms such as dry mucous membranes, tachycardia, hypotension, and oliguria. It can also lead to complications such as shock or kidney failure, which are serious but not as urgent as hypokalemia.
Choice D: Weight loss of 3% of total body weight. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Weight loss of 3% of total body weight indicates mild to moderate dehydration, which can be caused by fluid loss from vomiting and diarrhea. Weight loss can also reflect loss of muscle mass or fat tissue due to malnutrition or inflammation. Weight loss can affect the client’s nutritional status and immune function, but it is not as urgent as hypokalemia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
