A nurse is collecting data from a client who has a possible medical diagnosis of Guillain-Barré syndrome (GBS). Which of the following questions should the nurse ask the client?
"Have you had an MMR immunization?"
"Have you had a recent upper respiratory infection?"
"Have you traveled overseas recently?"
"Are you taking a multivitamin?"
The Correct Answer is B
A. "Have you had an MMR immunization?"
This question is not directly relevant to the assessment of Guillain-Barré syndrome. MMR immunization history may be pertinent to other health assessments, such as immunity to measles, mumps, and rubella.
B. "Have you had a recent upper respiratory infection?"
This is the correct answer. GBS often occurs after a recent upper respiratory or gastrointestinal infection, so asking about recent illnesses can provide valuable information for diagnosis.
C. "Have you traveled overseas recently?"
While travel history may be relevant to certain infectious diseases, it is not typically associated with the development of Guillain-Barré syndrome. Therefore, this question is less pertinent in this context.
D. "Are you taking a multivitamin?"
The use of multivitamins is unlikely to be directly related to the development of Guillain-Barré syndrome. While nutritional status is important for overall health, it is not a primary focus when assessing for GBS.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Withhold the next dose and notify the physician:
Withholding the next dose of the cholinergic agent is the appropriate immediate action because the presence of inspiratory and expiratory wheezing bilaterally suggests bronchoconstriction or bronchospasm, which can be a serious adverse reaction to the medication. Notifying the physician promptly allows for further assessment and management of the patient's respiratory symptoms. The physician may need to adjust the medication regimen, order diagnostic tests, or provide treatment for bronchoconstriction.
B. Give the next dose:
Administering the next dose of the cholinergic agent could worsen the patient's respiratory symptoms and exacerbate bronchoconstriction. This action is contraindicated in the presence of wheezing, as it may further compromise the patient's respiratory function.
C. Assess heart rate:
While assessing heart rate is an important aspect of patient assessment, it is not the priority in this scenario. The priority is to address the respiratory distress and potential bronchoconstriction associated with the cholinergic agent. Wheezing is a respiratory symptom that suggests airway obstruction, and immediate intervention is necessary to ensure adequate oxygenation and ventilation.
D. Assess blood pressure:
Similarly, while assessing blood pressure is important in patient care, it is not the priority in this situation. The priority is to address the respiratory distress and potential bronchoconstriction associated with the cholinergic agent. Wheezing indicates respiratory compromise, and prompt action is required to prevent further respiratory deterioration.
Correct Answer is C
Explanation
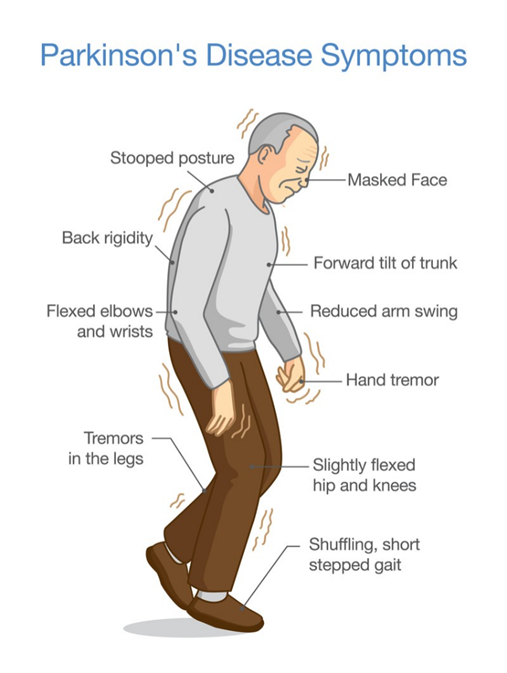
A. Increased blinking
Increased blinking is not a typical manifestation of bradykinesia. In fact, individuals with Parkinson's disease may experience reduced blinking (hypokinesia of blinking) rather than increased blinking.
B. States of euphoria
Euphoria is not typically associated with bradykinesia. Instead, individuals with Parkinson's disease may experience a range of mood changes, including depression, anxiety, or apathy, but euphoria is not a common finding.
C. Slurred speech
This is the correct answer. Slurred speech, or dysarthria, can occur in individuals with Parkinson's disease as a result of bradykinesia affecting the muscles involved in speech production. Bradykinesia can cause a reduction in the speed and coordination of movements necessary for clear speech, resulting in slurred or mumbled speech patterns.
D. Decreased respiratory rate
Decreased respiratory rate is not typically associated with bradykinesia. Bradykinesia primarily affects voluntary movements rather than involuntary processes such as respiration. While respiratory muscle weakness can occur in advanced stages of Parkinson's disease, it is not directly related to bradykinesia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
