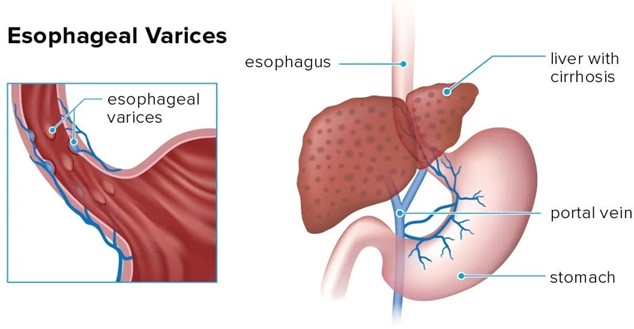
A nurse is caring for a client who was admited with bleeding esophageal varices and has an esophagogastric balloon tamponade with a Sengstaken-Blakemore tube to control the bleeding. Which of the following actions should the nurse take?
Provide frequent oral and nares care
Keep the client in a supine position
Ambulate the client four times per day
Encourage the client to consume clear liquids
The Correct Answer is A
Choice A: Provide frequent oral and nares care is the correct action for the nurse to take. Oral and nares care can help prevent infection, dryness, and irritation of the mucous membranes, which can be damaged by the pressure and friction of the tube. The nurse should also monitor the tube position, secure it with tape, and keep scissors at the bedside in case of emergency deflation.
Choice B: Keep the client in a supine position is not the correct action for the nurse to take. The supine position can increase the risk of aspiration, regurgitation, and gastric distension, which can worsen the bleeding and compromise the airway. The nurse should elevate the head of the bed to at least 30 degrees and use a semi-Fowler's or high-Fowler's position.
Choice C: Ambulating the client four times per day is not the correct action for the nurse to take. Ambulation can increase abdominal pressure and dislodge the tube, which can cause bleeding and perforation. The nurse should keep the client on bed rest and use passive range-of-motion exercises to prevent complications such as thromboembolism and muscle atrophy.
Choice D: Encouraging the client to consume clear liquids is not the correct action for the nurse to take. Clear liquids can increase gastric volume and acidity, which can aggravate the bleeding and interfere with hemostasis. The nurse should maintain a nothing-by-mouth status and provide intravenous fluids and nutrition as prescribed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
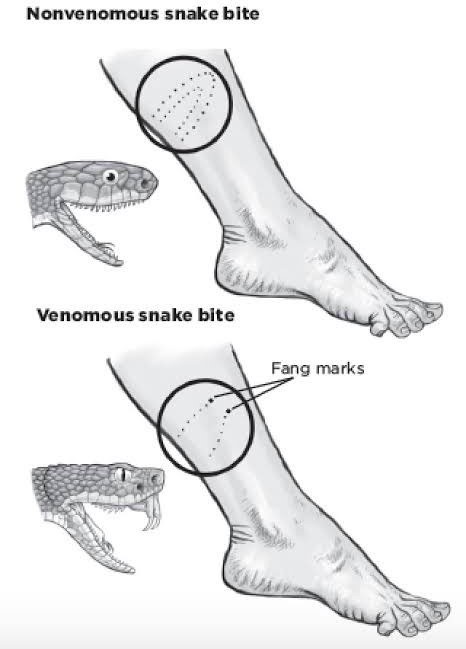
Correct Answer is C
Explanation
Choice A: Removing the elastic bandages is not recommended. These bandages help slow the spread of venom by compressing the lymphatic vessels. Removing them could worsen the envenomation.
Choice B: This is incorrect. The nurse should not discharge the client, as they may develop serious complications from the snake bite, such as swelling, bleeding, infection, or shock. The client should be monitored closely and treated accordingly.
Choice C: This is the correct action. Antivenom treatment is crucial for serious snake envenomation. The sooner it can be administered, the better the outcome.
Choice D: While pain management is important, it is not the priority in this situation. Antivenom takes precedence over pain medication.
Correct Answer is A
Explanation
Choice A: Troponin I is a laboratory test that the nurse should anticipate the provider to prescribe. Troponin I is a protein that is released into the blood when the heart muscle is damaged. Troponin I levels are elevated in clients who have acute myocardial infarction (AMI), which is a heart atack caused by a blockage of blood flow to the heart. Chest pressure and shortness of breath are common signs and symptoms of AMI. Troponin I is a specific and sensitive marker of cardiac injury and can help diagnose AMI and guide treatment.
Choice B: Aspartate aminotransferase (AST) is not a laboratory test that the nurse should anticipate the provider to prescribe. AST is an enzyme that is found in various tissues, such as the liver, heart, skeletal muscle, and kidneys. AST levels are elevated in clients who have liver damage, hepatitis, cirrhosis, or alcohol abuse. AST levels can also be elevated in clients who have AMI, but they are not as specific or sensitive as troponin I. AST is not a reliable indicator of cardiac injury and can be influenced by other factors.
Choice C: B-type natriuretic peptide (BNP) is not a laboratory test that the nurse should anticipate the provider to prescribe. BNP is a hormone that is secreted by the heart when it is stretched or overloaded. BNP levels are elevated in clients who have heart failure, which is a condition in which the heart cannot pump enough blood to meet the
body's needs. Shortness of breath can be a sign of heart failure, but chest pressure is not. BNP is not a specific or sensitive marker of cardiac injury and can be influenced by other factors.
Choice D: Lipase is not a laboratory test that the nurse should anticipate the provider to prescribe. Lipase is an enzyme that is produced by the pancreas and helps digest fats. Lipase levels are elevated in clients who have pancreatitis, which is an inflammation of the pancreas. Pancreatitis can cause abdominal pain, nausea, vomiting, and fever. Chest pressure and shortness of breath are not signs of pancreatitis. Lipase is not a specific or sensitive marker of cardiac injury and has no relation to AMI.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
