A nurse is caring for a client who is scheduled to undergo thoracentesis. In which of the following positions should the nurse place the client for the procedure?
Prone with arms raised over the head.
Sitting, leaning forward over the bedside table.
High Fowler's position
Side-lying with knees drawn up to the chest.
The Correct Answer is B
A. Prone with arms raised over the head.
This position involves lying face down with the arms raised over the head. It is not appropriate for thoracentesis because it does not provide easy access to the thoracic cavity, and it may compress the chest, making it difficult for the client to breathe comfortably during the procedure.
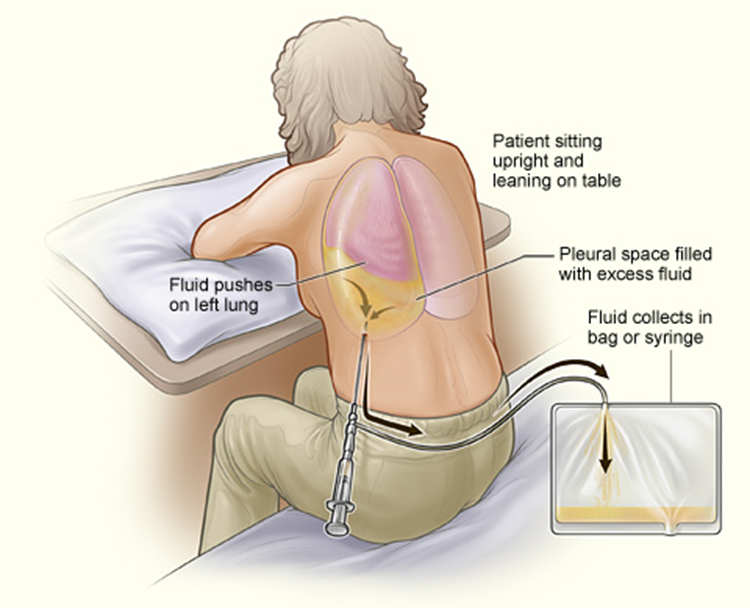
B. Sitting, leaning forward over the bedside table.
This is the correct choice. For thoracentesis, the client should be positioned sitting upright and leaning forward over the bedside table or supported by pillows. This position allows better access to the thoracic cavity and facilitates the removal of pleural fluid. Leaning forward also helps to open up the intercostal spaces, making it easier for the healthcare provider to insert the needle into the appropriate space between the ribs.
C. High Fowler's position.
The High Fowler's position involves the client sitting upright with the head of the bed elevated at a 90-degree angle. While this position may be used for other respiratory procedures or for comfort, it is not the optimal position for thoracentesis. It does not provide the same degree of access to the thoracic cavity as the sitting position with forward leaning.
D. Side-lying with knees drawn up to the chest.
This position involves lying on one side with the knees drawn up to the chest. It is not appropriate for thoracentesis because it does not provide access to the thoracic cavity, and it may obstruct the procedure. Additionally, this position may not be comfortable for the client during the procedure.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Air moves in and out of a wound in the chest wall.
In an open pneumothorax, also known as a sucking chest wound, there is a communication between the pleural space and the external environment through a wound in the chest wall. This allows air to move freely in and out of the pleural cavity during respiration. As a result, there is a loss of negative pressure within the pleural space, impairing lung expansion and leading to respiratory compromise. This condition is considered a medical emergency and requires prompt intervention to prevent tension pneumothorax and respiratory failure.
B. Air cannot pass freely into the thoracic cavity through a chest wound.
In an open pneumothorax, air can pass freely into the thoracic cavity through the chest wound. This communication between the external environment and the pleural space results in air movement in and out of the wound during respiration.
C. There are no audible sounds in an open pneumothorax.
In an open pneumothorax, there may be audible sounds, such as sucking or hissing sounds, particularly during inspiration. These sounds occur due to the movement of air in and out of the chest wound and can be indicative of the condition.
D. The air is trapped when it enters the cavity.
In an open pneumothorax, the air is not trapped when it enters the pleural cavity. Instead, air moves freely in and out of the wound in the chest wall, leading to respiratory compromise and potential progression to tension pneumothorax if left untreated.
Correct Answer is B
Explanation
A. Facial flushing
Facial flushing is not typically associated with atelectasis. Instead, it may occur in conditions such as oxygen toxicity or fever.
B. Increasing dyspnea
Atelectasis is a condition characterized by the collapse or partial collapse of a portion of the lung. Common findings in a client with atelectasis include increasing dyspnea (shortness of breath) due to impaired gas exchange and reduced lung function. As the affected lung tissue collapses, ventilation and oxygenation are compromised, leading to difficulty breathing.
C. Decreasing respiratory rate
A decreasing respiratory rate is not typically observed in a client with atelectasis. Instead, respiratory rate may increase as the body attempts to compensate for the impaired gas exchange and oxygenation resulting from lung collapse.
D. Dry cough
While coughing is a common symptom of atelectasis, it is typically associated with a productive cough rather than a dry cough. A dry cough is more commonly associated with conditions such as viral respiratory infections or allergic reactions. In atelectasis, the cough may be productive as the body attempts to clear mucus or other secretions from the affected airways.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
