A nurse is assessing a client who has asthma and signs of central cyanosis. Which of the following is a reliable indicator of cyanosis?
Oral mucosa
Tip of the nose
Ear lobes
Eye lids
The Correct Answer is A
A. Oral mucosa:
The oral mucosa, including the inside of the mouth, tongue, and lips, is a reliable indicator of cyanosis. Cyanosis appears as a bluish discoloration of these tissues due to decreased oxygen saturation in the arterial blood. Assessing the oral mucosa is an essential component of clinical examination, especially in patients with respiratory conditions like asthma, as it provides valuable information about oxygenation status.
B. Tip of the nose:
While the tip of the nose may exhibit cyanosis in some cases, it is not considered as reliable of an indicator as the oral mucosa. The nasal tip is more susceptible to external factors such as cold temperatures or poor circulation, which can cause temporary discoloration. Therefore, it may not always accurately reflect the oxygenation status of the patient compared to the oral mucosa.
C. Ear lobes:
Cyanosis may be observed in the ear lobes in cases of severe hypoxemia, but it is not as reliable of an indicator as the oral mucosa. The ear lobes are less commonly assessed for cyanosis compared to other areas such as the lips, nail beds, or oral mucosa. While cyanosis may be present in the ear lobes, it is not typically the primary site assessed for oxygenation status.
D. Eyelids:
Cyanosis is not typically observed in the eyelids and is not considered a reliable indicator of hypoxemia. The eyelids are not commonly assessed for cyanosis during clinical examinations. While the conjunctiva (the lining inside the eyelids) may appear pale in cases of severe anemia, it is not a specific sign of hypoxemia. Assessment of the oral mucosa, lips, and nail beds is preferred for evaluating oxygenation status in patients with respiratory conditions like asthma.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Place tissue soiled with respiratory secretions in a paper bag for later disposal:
This instruction is not accurate or recommended for managing tissue soiled with respiratory secretions, particularly in the context of tuberculosis (TB) infection. TB is transmitted through the air via respiratory droplets, so proper disposal of contaminated materials is crucial to prevent the spread of the infection. Instead of placing tissue in a paper bag, it should be disposed of in a sealed plastic bag to minimize the risk of transmission. Additionally, individuals with TB should be instructed on proper respiratory hygiene practices, such as covering their mouth and nose with a tissue or their elbow when coughing or sneezing, to prevent the spread of infectious droplets.
B. Provide samples for sputum cultures every 6 weeks:
Sputum cultures are an essential component of monitoring and managing tuberculosis (TB) treatment. However, obtaining samples every 6 weeks is not frequent enough, especially during the initial phase of treatment. In the early stages of TB treatment, sputum cultures are typically obtained more frequently, often weekly or biweekly, to monitor the response to treatment, assess for drug resistance, and ensure treatment effectiveness. As treatment progresses and the patient's condition stabilizes, the frequency of sputum cultures may be adjusted based on clinical judgment and guidelines.
C. Consume alcohol in moderation while taking antituberculosis medications:
Alcohol consumption is generally discouraged while taking antituberculosis medications. Some antituberculosis drugs, such as isoniazid and rifampin, can interact with alcohol and cause adverse effects, such as liver toxicity or drug metabolism issues. Therefore, individuals undergoing treatment for tuberculosis should be advised to abstain from alcohol consumption or limit it to a minimum to avoid potential complications. Providing instructions on alcohol consumption is an important aspect of tuberculosis management and medication adherence.
D. Wear a mask while out or around crowds of people:
This instruction is crucial for individuals with pulmonary tuberculosis to prevent the spread of the infection to others. Tuberculosis is transmitted through the air via respiratory droplets, particularly when an infected person coughs, sneezes, or talks. Wearing a mask while out or in crowded settings helps reduce the risk of transmitting infectious droplets to others and is an important infection control measure. It is especially important during the early stages of treatment when the individual is still infectious and shedding bacteria. Proper mask use, along with other respiratory hygiene practices, can help protect both the individual with tuberculosis and those around them from the spread of infection.
Correct Answer is B
Explanation
A. Prone with arms raised over the head.
This position involves lying face down with the arms raised over the head. It is not appropriate for thoracentesis because it does not provide easy access to the thoracic cavity, and it may compress the chest, making it difficult for the client to breathe comfortably during the procedure.
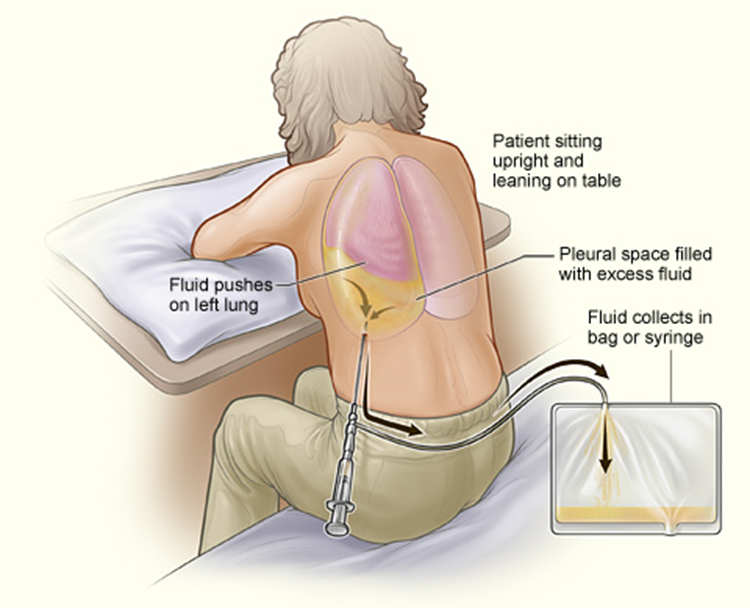
B. Sitting, leaning forward over the bedside table.
This is the correct choice. For thoracentesis, the client should be positioned sitting upright and leaning forward over the bedside table or supported by pillows. This position allows better access to the thoracic cavity and facilitates the removal of pleural fluid. Leaning forward also helps to open up the intercostal spaces, making it easier for the healthcare provider to insert the needle into the appropriate space between the ribs.
C. High Fowler's position.
The High Fowler's position involves the client sitting upright with the head of the bed elevated at a 90-degree angle. While this position may be used for other respiratory procedures or for comfort, it is not the optimal position for thoracentesis. It does not provide the same degree of access to the thoracic cavity as the sitting position with forward leaning.
D. Side-lying with knees drawn up to the chest.
This position involves lying on one side with the knees drawn up to the chest. It is not appropriate for thoracentesis because it does not provide access to the thoracic cavity, and it may obstruct the procedure. Additionally, this position may not be comfortable for the client during the procedure.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
