A patient has a diagnosis of Impaired Gas Exchange. Which assessment finding shows that the interventions have been effective?
The patient's Spo2 is 97% on 2L NC
The patient appears comfortable
The patient is coughing up copious white sputum
The patient is able to move out of bed without difficulty
The Correct Answer is A
A. The patient's Spo2 is 97% on 2L NC:
This assessment finding indicates that the patient's oxygen saturation level (SpO2) is 97% while receiving 2 liters per minute of oxygen via nasal cannula. Oxygen saturation is a measure of the percentage of hemoglobin saturated with oxygen in the blood. A SpO2 level of 97% suggests adequate oxygenation, which is essential for effective gas exchange. Therefore, if the patient's SpO2 is within the target range on the prescribed oxygen therapy, it indicates that the interventions aimed at improving gas exchange have been effective.
B. The patient appears comfortable:
While patient comfort is important, it is not a direct indicator of effective gas exchange. A patient may appear comfortable for various reasons, such as pain relief, proper positioning, or emotional support, but this does not necessarily reflect improved gas exchange. Therefore, while comfort is an important aspect of nursing care, it is not specifically indicative of the effectiveness of interventions for impaired gas exchange.
C. The patient is coughing up copious white sputum:
The presence of copious white sputum does not directly indicate improved gas exchange. White sputum may suggest various conditions, such as respiratory tract infections or inflammation, but it does not provide direct information about gas exchange efficiency. Effective gas exchange involves the exchange of oxygen and carbon dioxide at the alveolar-capillary membrane, which cannot be assessed solely based on sputum production.
D. The patient is able to move out of bed without difficulty:
The ability to move out of bed without difficulty may indicate improved overall physical function or mobility, but it does not specifically reflect improved gas exchange. Gas exchange primarily involves the transfer of oxygen from the alveoli into the bloodstream and the removal of carbon dioxide from the bloodstream into the alveoli for exhalation. While improved gas exchange may lead to enhanced physical endurance and reduced dyspnea, the ability to move out of bed without difficulty is not a direct measure of gas exchange efficiency.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
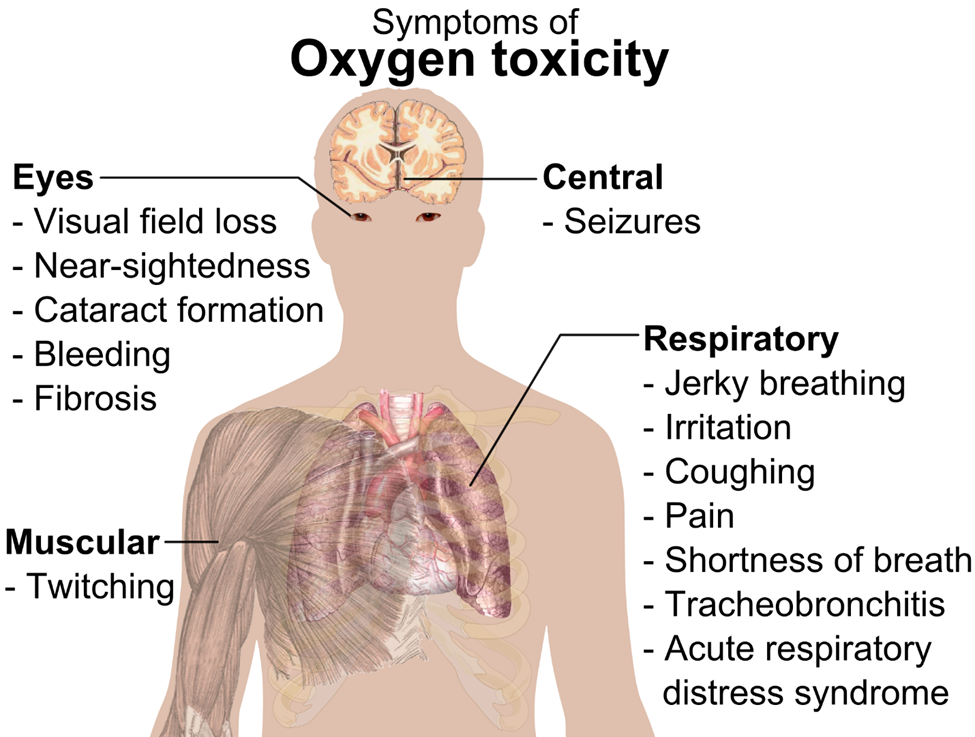
A. Muscle twitching
Muscle twitching is not a typical manifestation of oxygen toxicity. Instead, muscle twitching may be indicative of other conditions such as electrolyte imbalances (e.g., hypocalcemia or hypomagnesemia), neuromuscular disorders, or overstimulation of the nervous system.
B. Metallic taste in mouth
A metallic taste in the mouth is not commonly associated with oxygen toxicity. Instead, a metallic taste in the mouth may occur as a side effect of certain medications, dental issues, or as a symptom of other medical conditions such as acid reflux or oral infections.
C. Facial flushing
Facial flushing is a characteristic finding in oxygen toxicity. When exposed to high levels of oxygen over an extended period, individuals may experience facial flushing due to the vasodilatory effects of oxygen on blood vessels. This dilation of blood vessels leads to increased blood flow to the face, resulting in flushing or reddening of the skin.
D. Periorbital edema
Periorbital edema, or swelling around the eyes, is not a typical manifestation of oxygen toxicity. Instead, periorbital edema may occur as a result of various other conditions such as allergies, sinusitis, or fluid retention. It is not directly related to exposure to high levels of oxygen.
Correct Answer is A
Explanation
A. Fatigue
When collecting data from a client with pulmonary tuberculosis (TB), the nurse should expect to observe fatigue as one of the common manifestations. TB is a bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs. Fatigue is a typical symptom experienced by individuals with TB, often resulting from the body's immune response to the infection, as well as the systemic effects of inflammation and tissue damage caused by the bacteria.
B. High fever in the early morning
While fever is a symptom of tuberculosis, it may not necessarily occur specifically in the early morning. Fever associated with TB can occur at any time of the day and may persist for weeks to months. The pattern of fever can vary among individuals and may not consistently occur in the early morning.
C. Edema
Edema, or swelling due to fluid accumulation in tissues, is not typically associated with pulmonary tuberculosis. Edema is more commonly observed in conditions such as heart failure, renal failure, or liver disease, rather than in TB.
D. Increased appetite
Increased appetite is not a typical finding in pulmonary tuberculosis. In fact, individuals with active TB infection often experience appetite loss and unintended weight loss due to factors such as decreased food intake, metabolic changes, and systemic inflammation associated with the infection.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
