A nurse is caring for a client 2 hr following a spontaneous vaginal delivery and notes that the client has saturated two perineal pads with blood in a 30-min period. Which of the following actions should the nurse take first?
Check the consistency of the client's uterine fundus.
Have the client use the bedpan to urinate.
Increase the client's fluid intake.
Prepare to administer oxytocic medication.
The Correct Answer is A
Choice A reason:
Checking the consistency of the client's uterine fundus is the first action the nurse should take, as it can indicate the cause of excessive bleeding. A boggy or soft fundus indicates uterine atony, which is the most common cause of postpartum hemorrhage. The nurse should massage the fundus until it becomes firm and contracted.
Choice B reason:
Having the client use the bedpan to urinate is an important action, as a full bladder can displace the uterus and prevent it from contracting properly. However, this is not the first action the nurse should take, as it does not address the immediate source of bleeding.
Choice C reason:
Increasing the client's fluid intake is an important action, as it can help replace fluid loss and prevent hypovolemia and shock. However, this is not the first action the nurse should take, as it does not stop the bleeding.
Choice D reason:
Preparing to administer oxytocic medication is an important action, as it can stimulate uterine contractions and reduce bleeding. However, this is not the first action the nurse should take, as it requires a provider's prescription and may not be necessary if fundal massage is effective.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
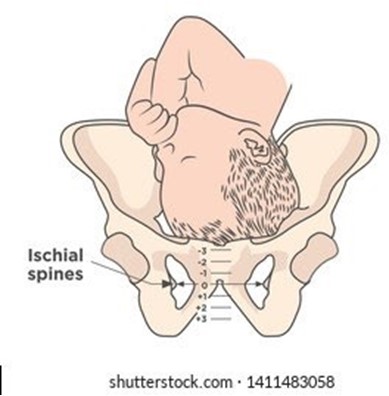
Choice A reason: The cervix is effaced 3 cm, it is dilated 30%, and the presenting part is 1 cm above the ischial spines is incorrect, as this does not follow the correct order and measurement of cervical assessment. Cervical effacement is measured in percentage, not in centimeters, and it indicates the thinning or shortening of the cervix. Cervical dilation is measured in centimeters, not in percentage, and it indicates the opening or widening of the cervix.
Choice B reason: The cervix is dilated 3 cm, it is effaced 30%, and the presenting part is 1 cm above the ischial spines is correct, as this follows the correct order and measurement of cervical assessment. Cervical dilation, effacement, and station are recorded in that order to describe the progress of labor. Station refers to the relationship between the presenting part of the fetus and the maternal pelvis, measured by the level of the ischial spines. A negative station means that the presenting part is above the spines, while a positive station means that it is below.
Choice C reason: The cervix is effaced 3 cm, it is dilated 30%, and the presenting part is 1 cm below the ischial spines is incorrect, as this does not follow the correct order and measurement of cervical assessment. Cervical effacement is measured in percentage, not in centimeters, and it indicates the thinning or shortening of the cervix. Cervical dilation is measured in centimeters, not in percentage, and it indicates the opening or widening of the cervix.
Choice D reason: The cervix is dilated 3 cm, it is effaced 30%, and the presenting part is 1 cm below the ischial spines is incorrect, as this does not match the documentation of station. A negative station means that the presenting part is above the spines, while a positive station means that it is below.
Correct Answer is C
Explanation
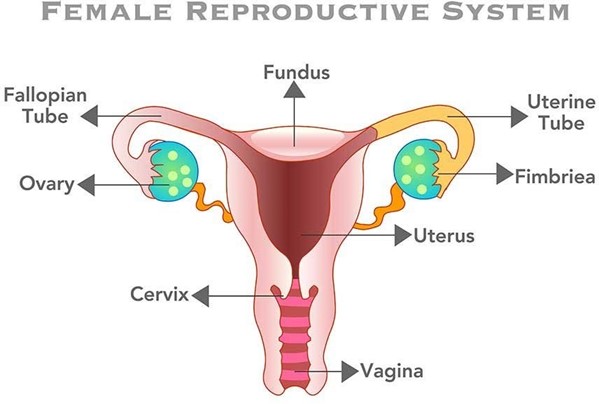
Choice A reason: Three fingerbreadths above the umbilicus is incorrect, as this position indicates a higher than expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one fingerbreadth per day. A high fundal height can indicate uterine atony, retained placental fragments, or bladder distension.
Choice B reason: One fingerbreadth above the symphysis pubis is incorrect, as this position indicates a lower than expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one finger-breadth per day. A low fundal height can indicate uterine inversion, which is a rare but life-threatening complication.
Choice C reason: At the level of the umbilicus is correct, as this position indicates a normal and expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one finger-breadth per day. A midline and firm fundus indicates adequate uterine contraction and involution.
Choice D reason: To the right of the umbilicus is incorrect, as this position indicates a deviated fundus for a client who is 12 hr postpartum. The fundus should be midline and not displaced to either side. A deviated fundus can indicate bladder distension, which can interfere with uterine contraction and involution. The nurse should assist the client to empty their bladder and reassess the fundal position.

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
