A nurse in the emergency department is caring for a client who has sustained a head injury. The nurse notes the client's IV fluids are infusing at 125 mL/hr. Which of the following is an appropriate action by the nurse?
Slow the rate to 50 mL/hr.
Increase the rate to 250 mL/hr.
Slow the rate to 20 mL/hr.
Continue the rate at 125 mL/hr.
The Correct Answer is C
Choice A Reason: This choice is incorrect because slowing the rate to 50 mL/hr may not be enough to prevent cerebral edema, which is a common complication of head injury. Cerebral edema is a swelling of the brain tissue due to increased fluid accumulation. It can cause increased intracranial pressure (ICP), which can lead to brain damage or death. Therefore, the nurse should limit the fluid intake of the client with head injury to avoid worsening the condition.
Choice B Reason: This choice is incorrect because increasing the rate to 250 mL/hr may cause fluid overload, which can also increase the ICP and worsen the cerebral edema. Fluid overload is a condition in which the body has too much fluid, which can impair the function of the heart, lungs, and kidneys. Therefore, the nurse should avoid giving too much fluid to the client with head injury.
Choice C Reason: This choice is correct because slowing the rate to 20 mL/hr may help to maintain adequate hydration and electrolyte balance, while preventing fluid overload and cerebral edema. This is a conservative approach that can be used until the client's neurological status and ICP are assessed and monitored.
Choice D Reason: This choice is incorrect because continuing the rate at 125 mL/hr may not be appropriate for the client with head injury, depending on their individual needs and condition. The nurse should adjust the fluid rate according to the client's vital signs, urine output, serum osmolality, and ICP. Therefore, the nurse should not assume that this rate is optimal for the client without further evaluation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","D","E"]
Explanation
Choice A Reason: This choice is incorrect because headache is not a common manifestation of ARF. Headache may be caused by various factors such as dehydration, stress, sinusitis, or migraine, but it does not indicate ARF.
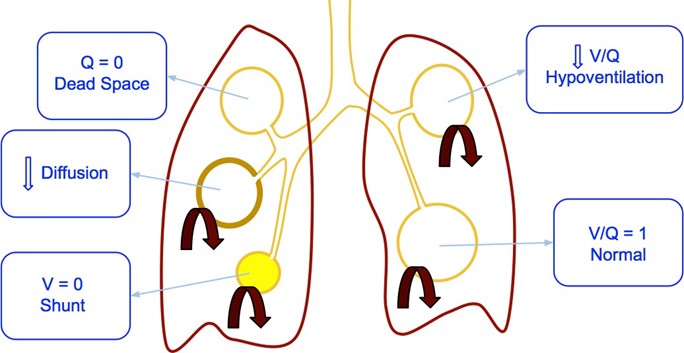
Choice B Reason: This choice is correct because severe dyspnea is a common manifestation of ARF. Dyspnea is a difficulty or discomfort in breathing that affects the oxygen delivery and carbon dioxide removal from the body. It may be caused by various factors such as lung disease, heart disease, anemia, or anxiety, but it indicates ARF when it is severe and persistent.
Choice C Reason: This choice is incorrect because nausea is not a common manifestation of ARF. Nausea is a sensation of uneasiness or discomfort in the stomach that may precede vomiting. It may be caused by various factors such as food poisoning, motion sickness, medication side effects, or pregnancy, but it does not indicate ARF.
Choice D Reason: This choice is correct because hypotension is a common manifestation of ARF. Hypotension is a condition in which the blood pressure is lower than normal (less than 90/60 mm Hg). It may be caused by various factors such as dehydration, blood loss, sepsis, or shock, but it indicates ARF when it is due to reduced cardiac output or vasodilation from hypoxia.
Choice E Reason: This choice is correct because decreased level of consciousness is a common manifestation of ARF. Decreased level of consciousness is a condition in which the person has impaired awareness or responsiveness to stimuli. It may be caused by various factors such as brain injury, stroke, seizure, or drug overdose, but it indicates ARF when it is due to increased carbon dioxide levels (hypercapnia) or decreased oxygen levels (hypoxemia) in the brain.
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because administering a nitrate antihypertensive is not the first action, as it may cause a rapid drop in blood pressure and worsen the client's condition.
Choice B Reason: This is incorrect because obtaining the client's heart rate is not the first action, as it does not address the cause of autonomic dysreflexia or relieve the symptoms.
Choice C Reason: This is incorrect because assessing the client for bladder distention is not the first action, as it may take time and delay the treatment of autonomic dysreflexia.
Choice D Reason: This is correct because placing the client in a high-Fowler's position is the first action, as it lowers the blood pressure by promoting venous return and reducing cardiac preload.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
