A home health nurse is caring for a child who has Lyme disease.
Which of the following is an appropriate action for the nurse to take?
Ensure the state health department has been notified.
Administer antitoxin
Educate the family to avoid sharing personal belongings.
Assess for skin necrosis
The Correct Answer is A
The correct answer is choice A. The nurse should ensure the state health department has been notified of the child’s Lyme disease, as it is a reportable disease in most states.
Reporting helps to monitor the incidence and prevalence of Lyme disease and to implement prevention and control measures.
Choice B is wrong because antitoxin is not used to treat Lyme disease.
Antitoxin is a substance that neutralizes the effects of a toxin, such as botulism or tetanus. Lyme disease is caused by a bacterium called Borrelia burgdorferi, which can be treated with antibiotics.
Choice C is wrong because Lyme disease is not transmitted by sharing personal belongings. Lyme disease is spread to humans by the bite of infected ticks that carry the
bacterium. The risk of getting Lyme disease can be reduced by avoiding tick-infested areas, wearing protective clothing, using insect repellent, and removing ticks promptly.
Choice D is wrong because skin necrosis is not a common complication of Lyme disease.
Skin necrosis is the death of skin tissue due to lack of blood supply or infection. Lyme disease can cause a characteristic skin rash called erythema migrans, which is usually circular or oval and expands over time. Other possible signs and symptoms of Lyme disease include fever, headache, fatigue, joint pain, and neurological problems.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The correct answer is choice A. Implement firm but flexible boundaries in their relationship.
This is because boundaries can help the client and family to respect each other’s roles, needs and preferences, and to avoid role confusion, resentment or guilt. Boundaries can also promote independence and self-care for the client, as well as prevent caregiver burnout for the family.
Choice B is wrong because minimizing open discussion regarding the changes can lead to misunderstanding, frustration or isolation. The client and family should communicate openly and honestly about their feelings, expectations and challenges, and seek support when needed.
Choice C is wrong because authoritative communication from the adult child can create a power imbalance, undermine the client’s autonomy and dignity, or cause conflict or resistance. The client and family should use respectful and collaborative communication, and involve the client in decision-making as much as possible.
Choice D is wrong because decreasing socialization with extended relatives can reduce the client and family’s support network, increase their stress or loneliness, or limit their opportunities for meaningful activities. The client and family should maintain contact with their relatives and friends, and participate in social or recreational activities that they enjoy.
Correct Answer is C
Explanation
Hyperthermia is a condition in which the body temperature is abnormally high, usually due to exposure to heat, infection, or certain medications.
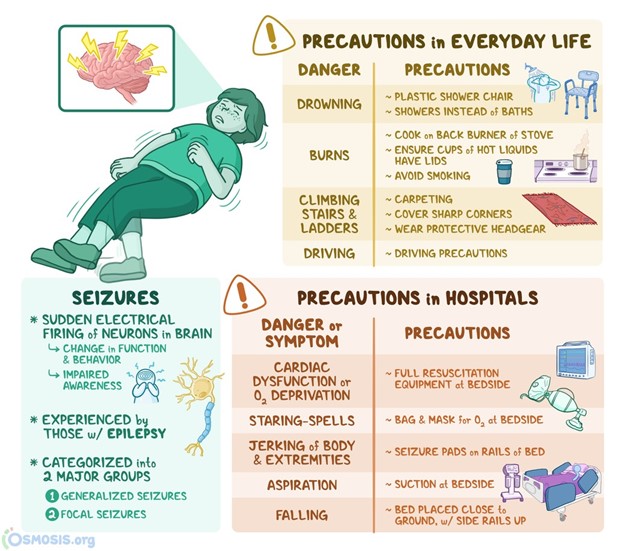
Hyperthermia can cause neurological complications, such as seizures, confusion, or coma. Therefore, the nurse should initiate seizure precautions for an adolescent who has hyperthermia to prevent injury and protect the airway.
Choice A is wrong because covering the adolescent with a thermal blanket would increase the body temperature and worsen hyperthermia. The nurse should remove excess clothing and use cooling measures, such as fans, ice packs, or cool fluids.
Choice B is wrong because submerging the adolescent’s feet in ice water would cause vasoconstriction and shivering, which would reduce heat loss and increase heat production. The nurse should avoid using extreme cold or ice water to cool the body.
Choice D is wrong because administering oral acetaminophen would not be effective for hyperthermia caused by non-infectious factors, such as heat exposure or medications.
Acetaminophen lowers the body temperature by reducing the hypothalamic set point, which is not altered in hyperthermia. Additionally, oral medications may be difficult to swallow or absorb in a hyperthermic patient.
Normal body temperature ranges from 36.5°C to 37.5°C (97.7°F to 99.5°F). Hyperthermia is defined as a body temperature above 38.5°C (101.3°F).
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
