A client with metastatic cancer reports a pain level of 10 on a scale of 0 to 10. Twenty minutes after the nurse administers an IV analgesic, the client reports no pain relief. Which intervention is most important for the nurse to include in this client's plan of care?
Replace transdermal analgesic patches every 72 hours.
Administer analgesics on a fixed and continuous schedule.
Monitor client for break through pain.
Frequently evaluate the client's pain.
The Correct Answer is C
C. Breakthrough pain is a transient exacerbation of pain that occurs despite the use of around- the-clock analgesics for persistent pain. Breakthrough pain episodes require rapid intervention with additional analgesics or adjustments to the current pain management regimen to provide adequate pain relief and improve the client's quality of life.
A. Replacing transdermal analgesic patches every 72 hours is important for ensuring consistent delivery of medication, but it is not directly related to addressing breakthrough pain.
B. Administering analgesics on a fixed and continuous schedule is important for maintaining baseline pain control, but it may not address breakthrough pain adequately.
D. Frequently evaluating the client's pain is essential, but monitoring specifically for breakthrough pain ensures timely intervention when pain exacerbations occur.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
C. The client's symptoms of weakness and palpitations are suggestive of hypoglycemia, a common complication in individuals with diabetes, particularly those on glucose-lowering medications such as insulin or sulfonylureas. Excessive perspiration, also known as diaphoresis, is a classic symptom of hypoglycemia and indicates the body's response to low blood sugar levels.
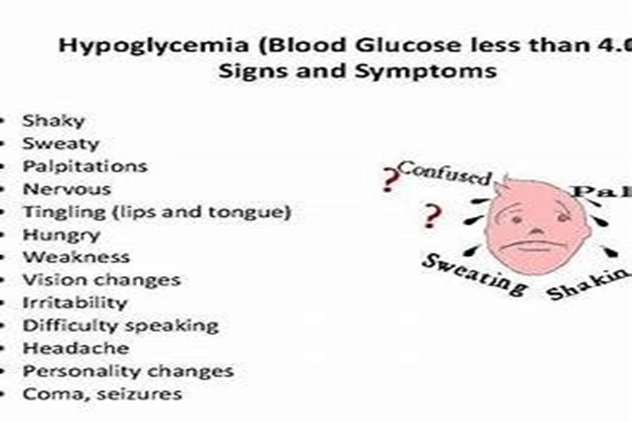
A. Cold extremities can be a sign of poor peripheral circulation, which may occur in individuals with diabetes, particularly in advanced stages or in the presence of peripheral vascular disease. However, it is not as specific to the acute episode of hypoglycemia
B. Myalgia (muscle pain) in the wrists and hands is not a typical symptom of hypoglycemia.
D. Dark yellow urine may indicate dehydration, which can occur in individuals with poorly controlled diabetes or during episodes of hyperglycemia. While dehydration is a concern in diabetes management, it is not directly related to the acute episode of hypoglycemia.
Correct Answer is D
Explanation
A. Releasing traction to use a bedpan may cause pain and discomfort to the client and risk exacerbating the fracture or compromising the alignment needed for surgery.
B. Log rolling the client and placing adult disposable briefs beneath them may not be suitable because it involves movement that can disrupt traction and worsen the client's pain.
Additionally, disposable briefs may not adequately manage urinary output, especially for a client awaiting surgery.
C.While using a catheter can be an option, it is generally not the first intervention unless the client is unable to void by other means or has a specific indication for catheterization. It carries risks, including infection, and should be considered carefully.
D. The nurse can assist the client in using a urinal while ensuring that traction is maintained. This allows the client to urinate without disrupting the traction setup, minimizing the risk of complications associated with the fracture.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
