While assisting a client to the toilet, the client begins to have a seizure and the nurse eases the client to the floor. The nurse calls for help and monitors the client until the seizing stops. Which intervention should the nurse implement first?
Observe for prolonged periods of apnea.
Observe for lacerations to the tongue.
Document details of the seizure activity.
Evaluate for evidence of incontinence.
The Correct Answer is A
A. This intervention is important for assessing the client's respiratory status during and after the seizure. Apnea can cause cardiac arrest and respiratory failure and hence a priority.
B. This intervention is crucial for assessing potential injury to the client's mouth or tongue, which can occur during a seizure due to involuntary muscle movements. However, before assessing for lacerations, the nurse should prioritize ensuring the client's safety.
C. Documenting details of the seizure activity is important for maintaining accurate medical records and providing information to the healthcare team. However, before documenting details of the seizure, the nurse should prioritize ensuring the client's safety and providing immediate assistance during the seizure. Therefore, while documentation is essential, it may not be the first intervention to implement.
D. While evaluating for incontinence is important for addressing the client's immediate needs and ensuring comfort, it may not be the first intervention to implement. The nurse should prioritize ensuring the client's safety and providing immediate assistance during the seizure.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
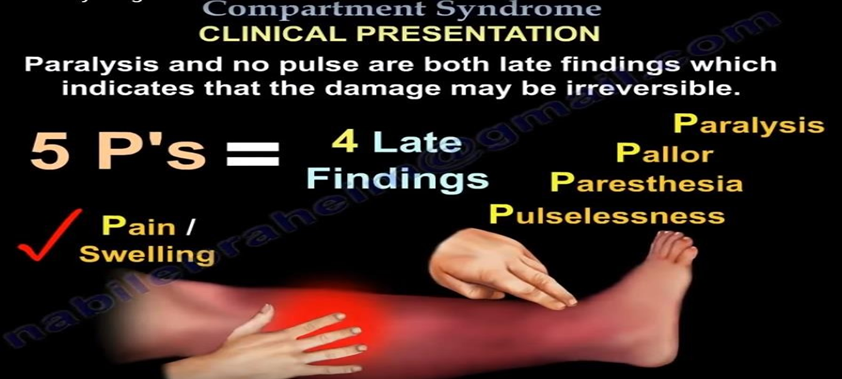
B. An increase in pain after cast placement could indicate complications such as compartment syndrome, which is a serious condition that occurs when increased pressure within a confined space (such as the area within the cast) compromises circulation and tissue perfusion. Assessing the radial pulse volume on the affected arm is crucial to evaluate perfusion distal to the fracture site.
A. Distraction technique may help manage the client's pain but does not address the underlying cause of the pain increase, which could be related to compromised circulation.
C. Analgesics relieve pain but do not address the immediate limb threatening issue at hand.
D. Measuring blood pressure is not directly related to assessing circulation distal to the fracture site.
Correct Answer is ["B","C","F"]
Explanation
B. Sugary beverages and juices are major sources of added sugars and can contribute to weight gain, insulin resistance, and an increased risk of type 2 diabetes mellitus. By eliminating these beverages from the diet, the client can reduce their intake of empty calories and excess sugars, which may help improve blood sugar control and reduce the risk of diabetes.
C. Fiber-rich foods, such as fruits, vegetables, whole grains, and legumes, can help improve blood sugar control, promote satiety, and support weight management. Fiber also helps regulate bowel movements and may reduce the risk of developing type 2 diabetes mellitus.
F. Refined grains, such as white bread, white rice, and sugary cereals, have been stripped of their fiber and nutrients during processing, leading to rapid spikes in blood sugar levels. Minimizing the intake of refined grains and opting for whole grains instead can help stabilize blood sugar levels, improve insulin sensitivity, and reduce the risk of type 2 diabetes mellitus.
A. While some studies have suggested that cinnamon may have beneficial effects on blood sugar control, the evidence is limited and inconsistent. Additionally, taking high doses of cinnamon supplements may not be safe for everyone, particularly those with liver disease or taking certain medications.
D. While reducing intake of unhealthy fats, such as saturated and trans fats, is important for overall health and reducing the risk of heart disease, eliminating all fats from the diet is unnecessary and potentially harmful. Healthy fats, such as those found in nuts, seeds, avocados, and olive oil, are essential for nutrient absorption, hormone production, and overall well-being.
E. Increasing protein intake significantly may not be necessary or advisable for this client, especially without knowing their specific dietary needs and preferences. While protein is an important macronutrient for muscle repair and maintenance, doubling the usual amount of protein in the diet may not offer additional benefits and could potentially lead to imbalances in other nutrients.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
