A client has an absolute neutrophil count (ANC) of 500/mm3 (0.5 x 10/L) after completing chemotherapy. Which intervention is most important for the nurse to implement? Reference Range:
Neutrophils (ANC) [2.500 to 5,800/mm (2.5 to 5.8 x 10/L)]
Review need for pneumococcal vaccine.
Implement bleeding precautions.
Place the client in protective isolation.
Assess vital signs every 4 hours.
The Correct Answer is C
C. An ANC of 500/mm3 (0.5 x 10/L) is indicative of severe neutropenia, which places the client at a significantly increased risk of developing infections due to the decreased ability of the immune system to fight off pathogens. Placing the client in protective isolation is essential to minimize the risk of exposure to infectious agents that could lead to severe infections
A. While reviewing the need for pneumococcal vaccine is important for preventing infections in immunocompromised clients, it may not be the most immediate priority in this scenario.
B. Implementing bleeding precautions is relevant for clients with thrombocytopenia but is not the most critical intervention for a client with severe neutropenia.
D. Assessing vital signs every 4 hours is a routine nursing intervention, but it may not directly address the heightened risk of infection associated with severe neutropenia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
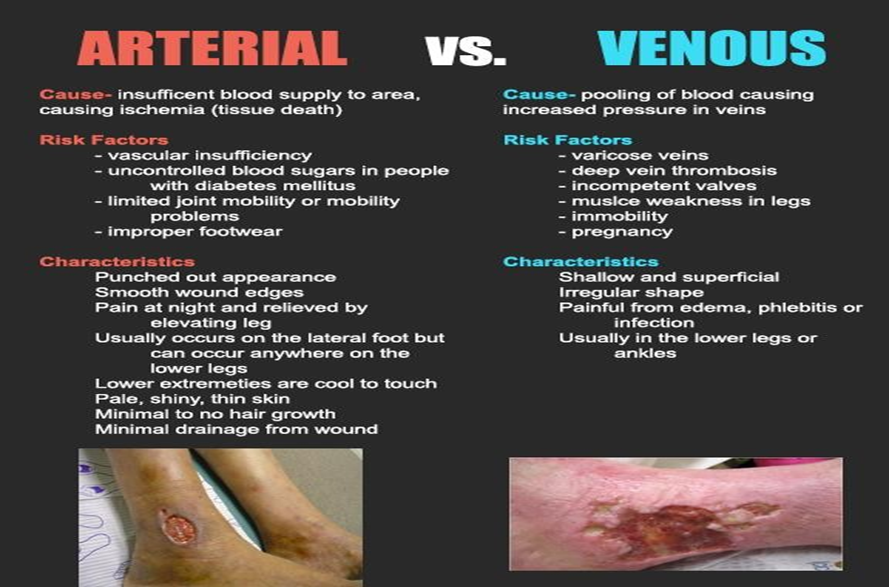
B. Severe edema is a common finding in venous insufficiency and is often present in the lower extremities. Venous hypertension leads to fluid leakage from capillaries, resulting in edema, which contributes to the development of venous ulcers. Venous ulcers typically have irregular shapes with irregular wound margins and may appear shallow or superficial.
A. Absent pedal pulses suggest arterial insufficiency, as reduced blood flow compromises peripheral circulation. Shiny skin, known as "thinning of the skin," is a characteristic finding in arterial insufficiency due to chronic ischemia and tissue hypoxia.
C. Hair loss on the lower extremities is a common finding in arterial insufficiency due to decreased blood flow to the hair follicles.
D. Black ulcers (gangrene) are indicative of tissue necrosis resulting from severe arterial insufficiency and lack of oxygen supply to the tissues. Dependent rubor refers to redness of the lower extremities when the legs are in a dependent position.
Correct Answer is C
Explanation
C. One of the hallmark features of ADC is the development of cognitive impairment, including changes in memory, concentration, and problem-solving abilities. The change in handwriting (graphomotor impairment) is a specific neurological symptom that may indicate cognitive dysfunction and is consistent with the diagnosis of AIDS dementia.
A. This symptom suggests emotional distress or mood disturbances, which can occur in individuals with HIV/AIDS due to the psychological impact of the diagnosis and the uncertainty surrounding the disease progression. However, it is not specific to AIDS dementia
B. Increased sleepiness or hypersomnia can occur in individuals with AIDS dementia due to disruptions in sleep-wake cycles and alterations in brain function. However, increased sleepiness alone is not specific to AIDS dementia
D. Social withdrawal or isolation can occur in individuals with HIV/AIDS due to various reasons, including stigma, depression, or physical symptoms. However, it is not specific to AIDS dementia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
