A client has urinary incontinence. Which assessment finding indicates that outcomes for a priority nursing diagnosis have been met?
The client reports drinking 8 to 9 glasses of water each day.
The client expresses satisfaction with undergarments for incontinence.
The family states that the client is more active and socializes more.
The skin in the perineal area is intact without redness upon inspection.
The Correct Answer is D
Choice A rationale:
While adequate hydration is important for overall health and urinary function, it does not directly address the priority nursing diagnosis of urinary incontinence. Increased fluid intake without addressing the underlying incontinence can actually exacerbate the problem by increasing urine output.
It's crucial to assess for signs of urinary retention or incomplete bladder emptying, as excessive fluid intake can worsen these conditions.
Individualized fluid intake goals should be established based on the client's overall health status, bladder capacity, and fluid balance.
Choice B rationale:
Satisfaction with incontinence products can improve comfort and quality of life, but it does not necessarily indicate that the underlying issue of incontinence has been resolved.
It's important to evaluate the effectiveness of incontinence products in managing leakage and preventing skin breakdown, but they should not be considered a definitive solution for incontinence.
Explore other interventions to address the root cause of incontinence, such as bladder training, pelvic floor muscle exercises, or medications.
Choice C rationale:
Increased activity and socialization can be positive outcomes of effective incontinence management, but they are not direct measures of the priority nursing diagnosis.
Improved social engagement and activity levels might reflect a reduction in incontinence episodes and increased confidence, but they should not be the sole indicators of success.
Assess for specific changes in incontinence frequency, severity, and impact on daily life to more accurately gauge progress.
Choice D rationale:
Intact, healthy skin in the perineal area is a direct and objective indicator that a priority nursing diagnosis of urinary incontinence has been met.
It demonstrates that the interventions implemented to manage incontinence have been effective in preventing skin breakdown and irritation, which are common complications of incontinence.
This finding aligns with the goal of maintaining skin integrity and preventing infection, which are essential aspects of incontinence care.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A rationale:
Uncompensated Respiratory Acidosis is characterized by a low pH (less than 7.35) and a high pCO2 (greater than 45 mmHg). In this case, the pH is slightly elevated (7.46), making this option less likely.
While the pCO2 is elevated (46 mmHg), the body has begun to compensate, as evidenced by the elevated HCO3 (29 mEq/L). This partial compensation does not align with an uncompensated respiratory acidosis.
Choice B rationale:
Compensated Metabolic Acidosis would present with a normal pH (7.35-7.45) due to full compensation by the respiratory system. In this case, the pH is slightly elevated (7.46), which is not consistent with full compensation.
Additionally, the HCO3 is elevated (29 mEq/L), which is characteristic of metabolic alkalosis, not acidosis.
Choice C rationale:
Partially Compensated Metabolic Alkalosis is the most likely interpretation based on the ABG results. The pH is elevated (7.46), indicating alkalosis.
The HCO3 is also elevated (29 mEq/L), which is the primary cause of metabolic alkalosis.
The pCO2 is elevated (46 mmHg), which is a compensatory mechanism to try to normalize the pH. However, the compensation is not complete, as the pH is still slightly elevated.
This partial compensation is consistent with partially compensated metabolic alkalosis.
Choice D rationale:
Partially Compensated Respiratory Acidosis would present with a low pH (less than 7.35) and an elevated pCO2 (greater than 45 mmHg).
The HCO3 would also be elevated, but to a lesser degree than in metabolic alkalosis, as it's a secondary compensatory mechanism.
In this case, the pH is slightly elevated (7.46), making respiratory acidosis less likely.
Correct Answer is A
Explanation
Choice A rationale:
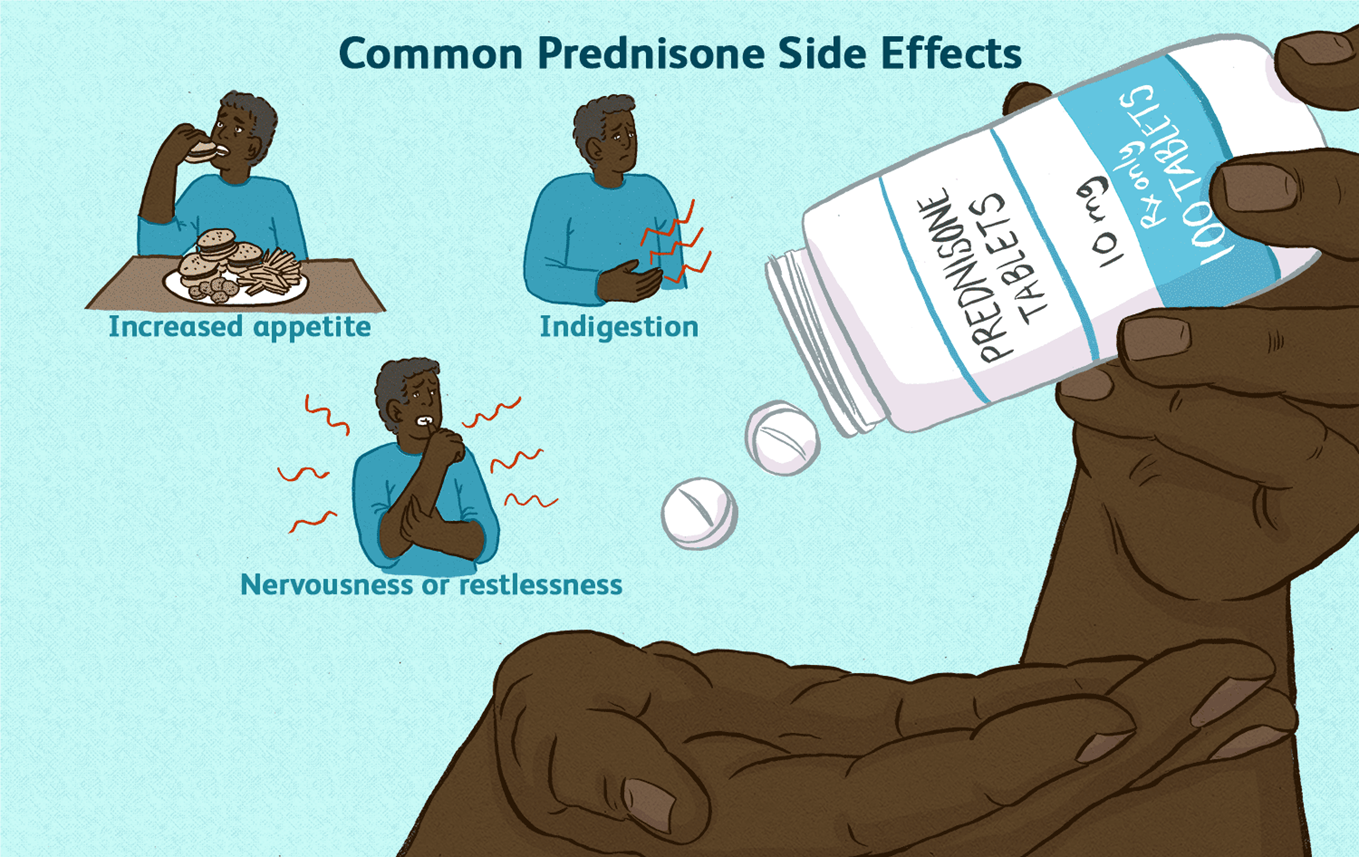
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
