A child with severe anemia requires a unit of red blood cells (RBCs). The nurse explains to the child that the transfusion is necessary to:
help her body stop bleeding by forming a clot
Fight the infection that she now has
Increase her energy so she will not be so tired
allows her parents to come visit her
The Correct Answer is C
Severe anemia is a condition characterized by a significant decrease in the number of red blood cells or hemoglobin in the blood, leading to reduced oxygen-carrying capacity. This can result in fatigue, weakness, and shortness of breath in the affected individual.
A red blood cell transfusion is given to a child with severe anemia to increase the number of red blood cells and, consequently, the hemoglobin level in the blood. This helps improve oxygen delivery to tissues and organs, which can lead to increased energy levels and reduced fatigue.
Option A is incorrect because red blood cell transfusion is not given to help the body stop bleeding by forming a clot. Platelets are responsible for clot formation, not red blood cells.
Option B is incorrect because a red blood cell transfusion is not used to fight infections. White blood cells and the immune system are responsible for fighting infections.
Option D is incorrect because a red blood cell transfusion is not given to allow her parents to come to visit her. Transfusions are medical treatments to address specific medical conditions and are not related to visitation rights.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["1250"]
Explanation
To calculate the daily fluid requirements for a child, you typically use the Holliday-Segar method, which provides guidelines based on the child's weight:
- For the first 10 kg of body weight, you give 100 ml per kg.
- For the second 10 kg of body weight, you give 50 ml per kg.
- For any weight above 20 kg, you give 20 ml per kg.
First, convert the child's weight from pounds to kilograms. To do this, divide the weight in pounds by 2.2.
For a child weighing 33 pounds:
- The weight in kilograms is approximately 15 kg (33 divided by 2.2).
Now, calculate the fluid requirement:
- For the first 10 kg of the child's weight, you need 1000 ml (10 kg multiplied by 100 ml).
- For the remaining 5 kg, you need 250 ml (5 kg multiplied by 50 ml).
Adding these together, the total daily fluid requirement is 1250 ml.
So, the daily fluid requirement for a child weighing 33 pounds is 1250 ml.
Correct Answer is C
Explanation
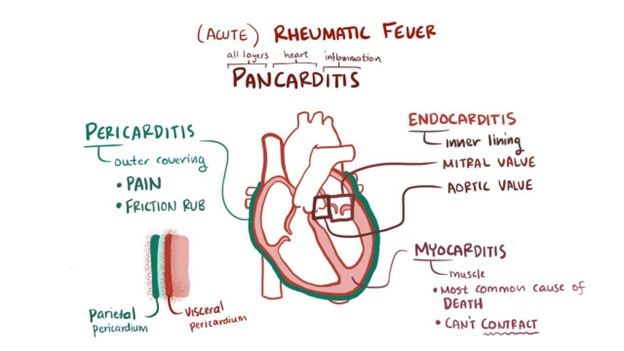
Rheumatic fever (RF) is a complication that can occur after an untreated or inadequately treated streptococcal throat infection (strep throat). It can affect the heart, joints, skin, and brain. One important aspect of managing RF is to prevent further episodes of strep throat, as it can trigger recurrent RF. Therefore, the child with a history of RF will require prophylactic antibiotics (usually penicillin or a related antibiotic) before certain invasive procedures, dental work, or surgeries to prevent strep throat and subsequent recurrence of RF.
Option A is not specific to rheumatic fever, and while electrolyte imbalances may be monitored and managed in certain cases of severe illness, it is not a core aspect of managing RF.
Option B is not accurate. While many children with RF do recover fully with appropriate treatment, they may be at risk of developing rheumatic heart disease, which can lead to long-term complications if not managed properly.
Option D is not a direct implication of RF. Rheumatic fever is not a genetically inherited condition, but a complication of strep throat caused by a bacterial infection. There is no evidence to suggest that having RF would directly affect the genetic implications for future offspring.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
