Hormonal Methods
A. Combined Oral Contraceptives (COCs) These pills contain estrogen and progestin, which work by:
1. Suppressing ovulation, which prevents the release of an egg from the ovaries.
2. Thickening cervical mucus, which blocks the entry of semen into the uterus.
3. Altering the uterine lining (decidua), which prevents the implantation of a fertilized egg.
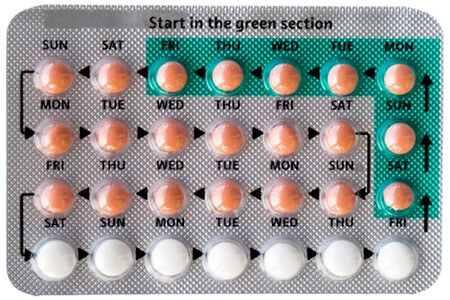
Some important points to remember when using COCs are:
• Routine Pap smears and breast examinations may be needed to check for any abnormalities.
• Consistent and proper use is essential for effectiveness. Follow the instructions on the package and do not skip any pills.
• Report any complications such as chest pain, shortness of breath (SOB), leg pain, headache, vision changes or high blood pressure (HTN) to your health care provider. These could be signs of serious side effects.
• If nausea occurs, take the pill at bedtime or with food.
Some benefits of using COCs are:
• They offer protection against endometrial, ovarian and colon cancer by reducing the exposure of these tissues to hormones.
• They reduce the incidence of benign breast disease, such as fibrocystic changes or lumps.
• They improve acne by lowering the levels of androgens (male hormones) in the body.
• They protect against the development of functional ovarian cysts, which are fluid-filled sacs that form on the ovaries.
Some risks of using COCs are:
• They increase the risk of blood clots (thromboembolism), stroke, heart attack and high blood pressure (HTN) by affecting the blood vessels and clotting factors.
• They increase the risk of gallbladder disease and liver tumors by stimulating the production and secretion of bile and liver enzymes.
• They exacerbate certain conditions such as migraine, epilepsy, asthma, kidney or heart disease by altering the levels of neurotransmitters and electrolytes in the body.
• Their effectiveness decreases when taking medications that affect liver enzymes, such as anticonvulsants (for seizures), antifungals (for fungal infections) or antibiotics (for bacterial infections). These drugs can increase the metabolism and clearance of COCs from the body.
B. Progestin-only Pills (minipill) These pills contain only progestin, which provides the same action as COCs by:
1. Decreasing the chances of fertilization by suppressing ovulation or altering cervical mucus.
2. Decreasing the chances of implantation by thinning or disrupting the uterine lining.
Some important points to remember when using minipills are:
• Another form of birth control may be needed during the first month of use to prevent pregnancy. This is because minipills take longer to become effective than COCs.
• Fewer adverse effects are associated with minipills than with COCs. This is because minipills do not contain estrogen, which is responsible for most of the side effects of COCs.
• Minipills are safer to take while breastfeeding than COCs. This is because minipills do not affect the quantity or quality of breast milk, unlike estrogen.
• Minipills are less effective than COCs. This is because minipills have a lower dose of progestin and a narrower window of time for taking them. If a pill is missed by more than three hours, backup contraception is needed for 48 hours.
• Increased occurrence of ovarian cysts may occur with minipills. This is because minipills do not suppress ovulation as effectively as COCs, which can lead to cyst formation on the ovaries.
• Breakthrough or irregular vaginal bleeding is the most common adverse effect of minipills. This is because minipills cause unpredictable changes in the uterine lining, which can result in spotting or bleeding between periods.
Some factors that decrease the effectiveness of minipills are:
• Taking medications that decrease liver function, such as rifampin (for tuberculosis) or ritonavir (for HIV). These drugs can reduce the absorption and efficacy of progestin in the body.
• Having certain medical conditions that contraindicate minipill use, such as bariatric surgery (weight loss surgery), lupus (an autoimmune disease), severe cirrhosis (liver damage), liver tumors or current or past breast cancer. These conditions can increase the risk of complications or interactions with progestin.
C. Emergency Contraceptive
o Emergency oral contraceptives should be taken within 72 hours after sex to prevent fertilization from taking place.
o They work by inhibiting ovulation and the transportation of sperm.
o An OTC antiemetic should be taken one hour before use, and if menstruation does not begin within 21 days, medical attention is required.
o A copper IUD can be used up to five days after sex for emergency contraception with a prescription.
o Emergency oral contraceptives and IUDs don't terminate an established pregnancy, and contraindicated for those who are already pregnant or have undiagnosed vaginal bleeding.
o The side effects of emergency oral contraception are nausea, heavier menstrual bleeding, lower abdomen pain, fatigue, and headache.
D. Transdermal Contraceptive Patch
o The transdermal contraceptive patch delivers estrogen and progesterone/progestin through the skin, inhibiting ovulation by thickening cervical mucus.
o It should be applied to dry skin on the butt, tummy, upper arm, or torso (except breast area).
o The patch should be replaced once a week and applied on the same day each week for three weeks, with no application on the fourth week.
o The contraceptive patch maintains consistent blood levels of hormones, avoids liver issues, and allows for swimming.
o However, it has the same adverse effects as oral contraceptives and increases the risk of Deep Vein Thrombosis (DVT) and venous thromboembolism slightly higher.
o Skin reactions and breast discomfort are also possible side effects.
o The contraceptive patch is contraindicated in the same cases as oral contraceptives and, it is less effective for people over 198lbs.
E. Injectable Progestins (Medroxyprogesterone)
Medroxyprogesterone is an intramuscular or subcutaneous injection given every 11-13 weeks. It inhibits ovulation and thickens cervical mucus. The injection should be started during the first five days of the menstrual cycle and repeated every 11-13 weeks thereafter. For postpartum non-breastfeeding, it should be administered within five days after delivery, and for breastfeeding mothers, it should be given in the sixth week postpartum.

Benefits of Injectable Progestins:
• Requires only four injections per year; Does not impair lactation; Possible absence of period and decreased bleeding; Decrease in uterine cancer risk (long-term use)
Adverse Effects of Injectable Progestins:
• Decreased bone mineral density; Weight gain; Depression; Irregular vaginal spotting; Return to fertility can be delayed for up to 18 months after discontinuation
Contraindications of Injectable Progestins:
• Breast cancer; Cardiovascular disease; Abnormal liver function; Liver tumors; Unexplained vaginal bleeding
• Can impair glucose tolerance for patients with Diabetes Mellitus (DM) and increase diabetes risk
Additional Information on Injectable Progestins:
• Calcium intake and weight-bearing exercise are recommended to prevent osteoporosis
• Do not massage the injection site.
F. Contraceptive Vaginal Ring (Etonogestrel and Ethinyl Estradiol)
The contraceptive vaginal ring is a flexible silicone ring containing etonogestrel and ethinyl estradiol. It should be replaced after three weeks, and a new ring should be inserted within seven days. It should be inserted on the same day of the week each month. If removed for more than four hours, a new ring should be inserted, and a barrier method should be used for seven days.
Benefits:
• Doesn't have to be fitted
• Route increases bioavailability of hormones (lower dose, reducing adverse effects)
Adverse Effects:
• Blood clots; Hypertension (HTN); Stroke; Myocardial Infarction (MI); Vaginal irritation/discomfort; Increased vaginal secretions; Same adverse effects as oral contraceptives; Some users report discomfort during sex (the ring can be removed for up to three hours without compromising effectiveness)
• Prescription required
G. Implantable Progestin
The implantable progestin consists of thin rods of progestin implanted under the skin of the inner upper arm. It suppresses the ovulatory cycle and thickens cervical mucus. Patients should avoid trauma to the area and use condoms for protection from sexually transmitted infections (STIs).
Benefits:
• Continuous for three years
• Reversible
• Inserted immediately after spontaneous/elective abortion, childbirth, while breastfeeding
Adverse Effects:
• Irregular unpredictable menstruation; Mood changes; Headache; Acne; Depression; Decreased bone density; Weight gain; Scarring at the site warrants the need for removal
Contraindications:
• Unexplained vaginal bleeding
• Infection at the site
Additional Information:
• Increased risk for ectopic pregnancy
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Questions on Hormonal Methods
Correct Answer is A
Explanation
Correct Answer is C
Explanation
Correct Answer is C
Explanation
Search Here
Related Topics
More on Nursing
- Newborn Complications
- Physiological And Physical Changes In Pregnancy
- Prenatal Diagnostic Tests And Procedures
- Pre-eclampsia, Eclampsia
- Pre-term Labor
- Prolonged and Obstructed Labor and Ruptured Uterus
- Phases of Maternal Role Attainment
- Postpartum Depression
- Postpartum Disorders: DVT, Pulmonary Embolism
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
