Which of the following arrhythmias is associated with heart failure?
First-degree heart block
Atrial fibrillation
Ventricular tachycardia
Sinus bradycardia
Correct Answer : B,C
Choice A Reason:
First-degree heart block is a condition where the electrical signals in the heart are delayed but still reach the ventricles. It is generally considered benign and does not typically lead to heart failure. It is often asymptomatic and discovered incidentally on an ECG.
Choice B Reason:
Atrial fibrillation (AFib) is a common arrhythmia associated with heart failure. AFib causes the atria to beat irregularly and often rapidly, which can lead to poor blood flow and increased risk of stroke. In heart failure patients, AFib can exacerbate symptoms and worsen the prognosis due to the loss of atrial contraction and irregular ventricular response.
Choice C Reason:
Ventricular tachycardia (VT) is a serious arrhythmia that is often associated with heart failure. VT originates in the ventricles and can lead to hemodynamic instability and sudden cardiac death if not treated promptly. It is a common complication in patients with heart failure and cardiomyopathy.
Choice D Reason:
Sinus bradycardia is a slower than normal heart rate, typically less than 60 beats per minute. While it can occur in healthy individuals, especially athletes, it is not specifically associated with heart failure. In some cases, severe bradycardia can lead to symptoms of heart failure, but it is not a primary arrhythmia linked to the condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Monitoring the client for an elevated temperature is crucial because it can indicate an infection at the pin sites or other complications. Infections are a common risk with halo fixation devices due to the invasive nature of the pins.
Choice B Reason:
Ensuring the halo jacket is snug against the client's skin is incorrect. The halo jacket should fit properly but not be too tight, as this can cause skin breakdown and discomfort. There should be enough space to insert a flat hand between the vest and the skin.
Choice C Reason:
Providing range of motion to the client's neck is not appropriate for a client with a halo fixation device. The purpose of the halo is to immobilize the neck to allow for proper healing of cervical injuries. Any movement could jeopardize the stability of the injury.
Choice D Reason:
Removing the vest daily to inspect the client's skin integrity is incorrect. The halo vest should not be removed frequently as it is meant to provide continuous immobilization. Skin integrity can be monitored by checking the areas around the vest without removing it.
Correct Answer is ["A","D"]
Explanation
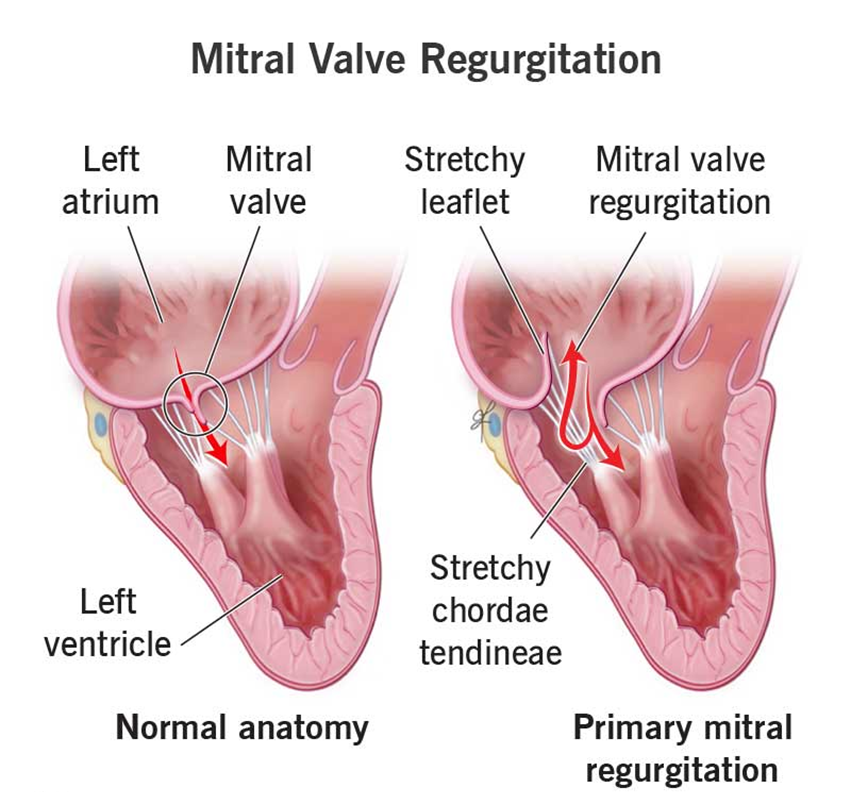
Choice A Reason:
Neck vein distention is a common finding in patients with mitral valve insufficiency. This condition leads to increased pressure in the left atrium, which can back up into the pulmonary veins and subsequently the right side of the heart, causing jugular venous distention.
Choice B Reason:
Splenomegaly is not typically associated with mitral valve insufficiency. It is more commonly seen in conditions like liver disease, hematologic disorders, and infections. Mitral valve insufficiency primarily affects the heart and lungs rather than the spleen.
Choice C Reason:
Petechiae are small, red or purple spots caused by bleeding into the skin. They are not a common finding in mitral valve insufficiency. Petechiae are more often associated with conditions that affect platelet function or coagulation, such as thrombocytopenia or vasculitis.
Choice D Reason:
An S4 heart sound, also known as an atrial gallop, can be heard in patients with mitral valve insufficiency. This sound occurs due to the atria contracting forcefully to overcome a stiff or hypertrophic ventricle, which is often a result of chronic pressure overload from the regurgitant flow.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
