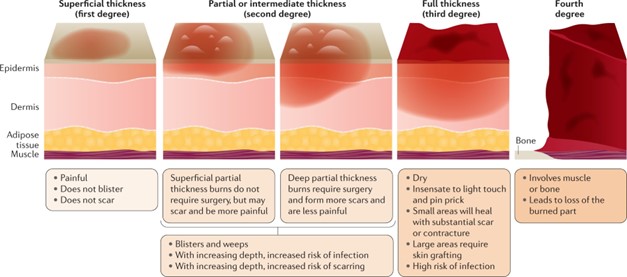
When caring for a client with full-thickness burns to both lower extremities, which assessment finding(s) warrant immediate intervention by the nurse? (Select all that apply.)
Sloughing tissue around wound edges.
Change in the quality of the peripheral pulses.
Weeping serosanguineous fluid from wounds.
Loss of sensation to the left lower extremity.
Complaint of increased pain and pressure.
Correct Answer : B,D,E
These findings suggest potential complications and compromise to the client's circulation and nerve function, which require immediate attention.
Changes in the quality of peripheral pulses indicate alterations in blood flow and may suggest vascular compromise or decreased perfusion to the affected areas. This finding requires immediate intervention to prevent further damage and ensure adequate blood supply to the extremities.
Loss of sensation to the left lower extremity can be indicative of nerve injury or impaired peripheral nerve function. It is important to assess for nerve damage and address it promptly to prevent complications and maximize the client's recovery.
Complaints of increased pain and pressure are concerning because they may indicate the development of compartment syndrome, a serious complication in which pressure within the muscles and tissues builds up to dangerous levels. Prompt intervention is necessary to relieve the pressure and prevent tissue damage.
While sloughing tissue around wound edges and weeping serosanguineous fluid from wounds are important assessment findings in the context of burn care, they do not require immediate intervention compared to the findings mentioned above. These findings should still be addressed and managed appropriately, but they are not considered immediate emergencies.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
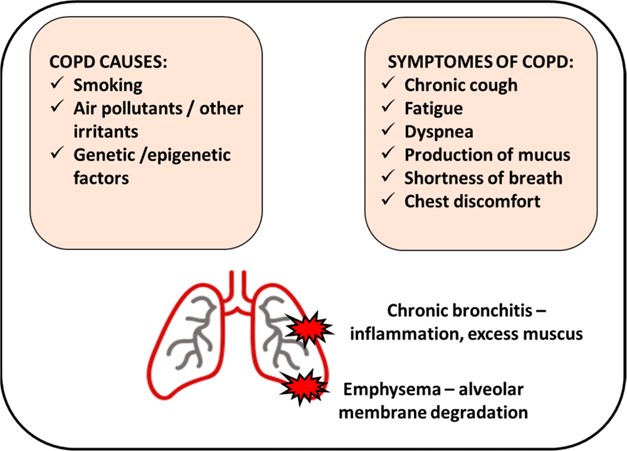
Emphysema is a chronic obstructive pulmonary disease (COPD) characterized by the destruction of lung tissue and loss of elasticity in the alveoli. This leads to poor gas exchange, specifically the reduced ability of oxygen to enter the bloodstream and carbon dioxide to be eliminated from the body. Impaired gas exchange can result in hypoxemia and hypercapnia, leading to symptoms such as shortness of breath, fatigue, and decreased exercise tolerance.
While self-care deficit, activity intolerance, and ineffective airway clearance are all potential complications associated with emphysema, impaired gas exchange is the priority due to its direct impact on the client's oxygenation and overall respiratory function.
Addressing impaired gas exchange and optimizing oxygenation is essential to support the client's respiratory health and prevent further complications. Management strategies for impaired gas exchange may include administering supplemental oxygen, implementing respiratory treatments to improve lung function, and providing education on breathing techniques and energy conservation.
Correct Answer is {"A":{"answers":"A"},"B":{"answers":"B"},"C":{"answers":"A"},"D":{"answers":"A"},"E":{"answers":"B"}}
Explanation
A. Understanding: The client recognizes that taking allergy medications before the hike might have helped prevent an exacerbation.
B. No understanding: The client doesn't realize that eating a snack could impact asthma symptoms. Proper education is needed here.
C. Understanding: The client acknowledges that exposure to cigarette smoke during the hike could have contributed to the exacerbation.
D. Understanding: The client identifies that stress management could be important in preventing asthma exacerbations.
E. No understanding: The client is not aware that taking an extra dose of Fluticasone-Salmeterol could have been beneficial. Further education is necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
