A client with a history of lung cancer reluctantly comes to the clinic because of persistent hoarseness and a chronic cough. The client's respirations are labored when speaking and the capillary refill is 3 seconds. Which additional finding warrants intervention by the nurse?
Coarse breath sounds.
Rust colored sputum.
Unexplained fatigue.
Clubbed fingernails.
The Correct Answer is A
The client's history of lung cancer, persistent hoarseness, chronic cough, and labored respirations when speaking indicate potential respiratory complications. Coarse breath sounds may suggest the presence of airway obstruction or fluid accumulation in the lungs, which can be indicative of a worsening condition.
The nurse should intervene promptly by assessing the client's respiratory status further, providing appropriate respiratory support, and notifying the healthcare provider for further evaluation and intervention.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
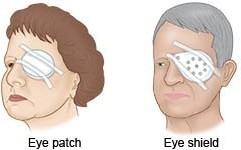
After retinal detachment surgery, it is crucial to protect the eye and the surgical repair site from accidental trauma or pressure. Providing an eye shield helps to shield the eye during sleep when the client may not have conscious control over their movements.
This can help prevent inadvertent rubbing or bumping of the eye, which could potentially disrupt the surgical repair and hinder the healing process.
Obtaining vital signs every 2 hours during hospitalization is a routine nursing intervention for postoperative care in general but is not specific to retinal detachment surgery. The frequency of vital sign monitoring may vary depending on the client's overall condition and the healthcare provider's orders.
Teaching a family member to administer eye drops may be necessary for the client's ongoing care, but it is not specifically related to the immediate postoperative period. Eye drop administration instructions can be provided as part of the client's discharge teaching.
Encouraging deep breathing and coughing exercises is a general postoperative intervention that promotes respiratory function and helps prevent complications such as pneumonia. While important for overall postoperative care, it is not specific to retinal detachment surgery.
Correct Answer is D
Explanation
The ability to effectively communicate and provide accurate information can be impacted by external factors such as noise, distractions, or an unfamiliar environment. By assessing the surroundings, the nurse can identify and address any potential barriers to communication.
Once the nurse has addressed any environmental factors that may be hindering communication, they can proceed with other strategies to facilitate the health history assessment. This may include providing a printed healthcare assessment form to assist the client in organizing their thoughts or deferring the assessment until the client is less anxious.
Asking the family member to answer the questions should be considered if the client is unable to provide accurate information or is cognitively impaired. However, it is important to first address any environmental factors and attempt to engage the client directly in the assessment process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
