The nurse is caring for a client after a thoracentesis that drained 50 mL of clear fluid from the left lung. Which assessment finding should the nurse report to the healthcare provider immediately?
Dullness bilaterally on percussion.
Serosanguinous drainage from the chest tube.
Diminished breath sounds in the left lower lobe.
Mediastinal shift to the right.
The Correct Answer is D
A) Incorrect- Dullness bilaterally on percussion is not a normal finding, but it is not an immediate concern after thoracentesis. It may indicate fluid accumulation or consolidation in both lungs, which could be related to other conditions such as pneumonia or heart failure.
B) Incorrect- Serosanguinous drainage from the chest tube is expected after thoracentesis, as long as it is not excessive or continuous. The nurse should monitor the amount and color of the drainage and document it accordingly.
C) Incorrect- Diminished breath sounds in the left lower lobe are also expected after thoracentesis, as the procedure removes fluid and air from the pleural space and reduces lung expansion. The nurse should auscultate the lungs before and after the procedure and compare the findings. The breath sounds should improve gradually as the lung re-expands.
D) Correct- This is a sign of tension pneumothorax, which is a life-threatening complication of thoracentesis. Tension pneumothorax occurs when air accumulates in the pleural space and creates positive pressure that pushes the mediastinum (the heart, great vessels, and trachea) to the opposite side of the chest. This can impair venous return, cardiac output, and respiratory function. The nurse should report this finding to the healthcare provider immediately and prepare to assist with needle decompression or chest tube insertion.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
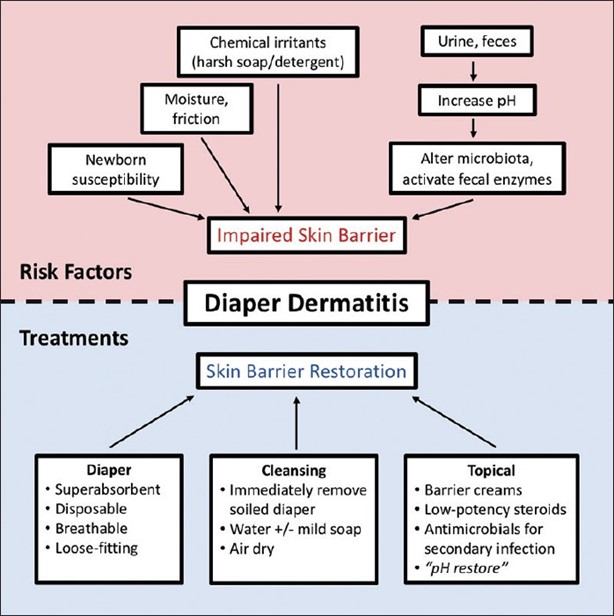
The excoriated and red skin in the diaper area suggests the presence of diaper dermatitis, which is commonly caused by prolonged exposure to moisture and irritants such as urine and feces. Changing the diaper more frequently helps to minimize the exposure to these irritants and promotes better skin hygiene.
Asking the mother to decrease the infant's intake of fruits for 24 hours is not necessary unless there is evidence of diarrhea or specific dietary concerns. Fruits are generally a healthy part of an infant's diet and do not directly cause diaper dermatitis.
Encouraging the mother to apply lotion with each diaper change may not be recommended in this case, as lotions and creams can further trap moisture and exacerbate the condition. It is best to keep the area clean and dry.
Telling the mother to cleanse with soap and water at each diaper change may be too harsh for the infant's sensitive skin. Plain water or mild, fragrance-free wipes are typically sufficient for cleaning the diaper area. Soap can be drying and irritating to the skin, so it is generally not necessary unless there is a specific indication.
Correct Answer is B
Explanation
Febuxostat is a medication used to manage hyperuricemia and prevent gout attacks. However, it has been associated with hepatotoxicity, including liver enzyme elevations and liver failure. Therefore, it is important for the nurse to instruct the client to report any signs or symptoms of liver dysfunction, such as right upper quadrant discomfort. This will allow for prompt evaluation and appropriate management if hepatotoxicity occurs.
While maintaining a healthy weight and dietary modifications may be beneficial for managing gout, specific instructions regarding protein intake should be individualized and provided by a healthcare provider or a registered dietitian.
Using an electric heating pad when pain is at its worst may provide temporary symptomatic relief for gout attacks, but it is not specific to the use of febuxostat. The focus of discharge teaching should be on medication adherence, monitoring for adverse effects, and lifestyle modifications to prevent gout attacks.
Replacing dietary table salt with salt substitutes is not a specific instruction for a client taking febuxostat. While reducing sodium intake may be recommended as part of an overall healthy diet, it is not directly related to the use of febuxostat or management of gout attacks. Dietary modifications for gout management should be individualized and based on the client's specific needs and preferences.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
