The nurse is assessing a patient's postoperative wound and finds it has separated from the suture line with extrusion of the intestine through the opening. How does the nurse document this finding?
Wound evisceration
Wound dehiscence
Wound infection
Wound tunneling
The Correct Answer is A
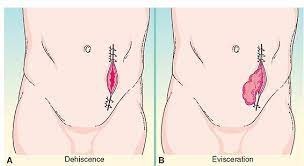
Wound evisceration refers to the protrusion of internal organs or tissues through an open wound. In this case, with the separation of the wound and extrusion of the intestine through the opening, it is a clear indication of wound evisceration. It is a surgical emergency that requires immediate medical attention.
Wound dehiscence, on the other hand, refers to the separation or opening of a previously closed surgical incision or wound. It does not involve the extrusion of internal organs or tissues.
Wound infection refers to the presence of infectious microorganisms in the wound, leading to inflammation and other signs of infection.
Wound tunneling refers to the formation of narrow channels or tunnels within the wound, often caused by improper wound healing or infection.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
According to the given information, Aydan's insulin lispro (Humalog) dosage is 1 unit per 50 grams of carbohydrates eaten. As Aydan has just consumed 150 grams of carbs for lunch, we can calculate the insulin dose as follows:
Insulin dose = Carbohydrates eaten / Insulin-to-carbohydrate ratio Insulin dose = 150 grams / 50 grams/unit
Insulin dose = 3 units
Therefore, the nurse should prepare to administer 3 units of Aydan's prescribed rapid-acting insulin (Insulin lispro) to cover the carbohydrates he consumed for lunch. The long-acting insulin (Glargine) is typically given at bedtime to provide a basal insulin level and is not directly related to meal coverage.
Correct Answer is B
Explanation
Opioid tolerance occurs when the body becomes less responsive to the effects of opioids over time. This means that higher doses of the medication are needed to achieve the same level of pain relief that was previously achieved with lower doses. Opioid tolerance is a common phenomenon in long-term opioid therapy and can occur in patients who have been using opioids for an extended period.
Opioid abstinence syndrome, also known as opioid withdrawal, refers to the set of symptoms that occur when a person abruptly stops or reduces their use of opioids after developing physical dependence.
Opioid toxicity refers to the harmful effects that occur when an individual takes an excessive dose of opioids, leading to potentially life-threatening complications. It is characterized by symptoms such as respiratory depression, sedation, pinpoint pupils, and decreased level of consciousness.
Opioid addiction is a complex condition characterized by compulsive drug-seeking behavior, loss of control over opioid use, and continued use despite negative consequences.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
