The final step in the formation of a blood clot is:
The formation of prothrombin activator.
The conversion of prothrombin to thrombin by prothrombin activator.
The conversion of fibrinogen to fibrin by thrombin.
Tissue damage.
The Correct Answer is C
The conversion of fibrinogen to fibrin by thrombin is the final step in the formation of a blood clot.
Fibrin is a protein that forms a net-like structure that traps platelets and other blood cells, making the clot stronger and more durable.
Choice A is wrong because the formation of a prothrombin activator is the first step in the formation of a blood clot.
A prothrombin activator is a complex of enzymes that converts prothrombin to thrombin.
Choice B is wrong because the conversion of prothrombin to thrombin by the prothrombin activator is the second step in the formation of a blood clot.
Thrombin is an enzyme that converts fibrinogen to fibrin.
Choice D is wrong because tissue damage is not a step in the formation of a blood clot, but a trigger for the clotting process.
When blood vessels are injured, they release substances that activate platelets and clotting factors.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Atrial natriuretic peptide (ANP) is a hormone secreted by the heart when the atria are stretched by high blood pressure or volume.
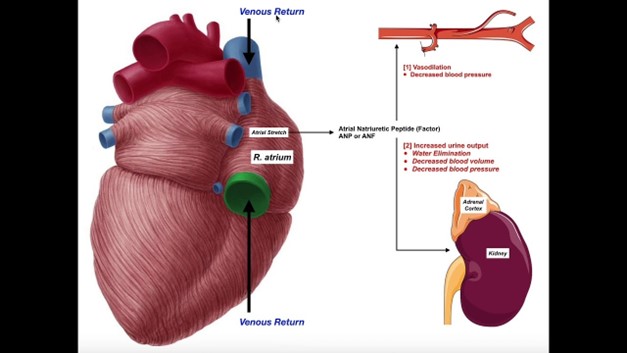
ANP has multiple effects, such as increasing urine and salt excretion, lowering blood pressure, and opposing the renin-angiotensin-aldosterone system.
Therefore, ANP inhibits the release of renin and aldosterone, which are hormones that increase blood pressure and sodium retention.
Choice A is wrong because ANP is not released from the adrenal cortex but from the cardiac atria.
ANP does not stimulate atrial hormones but rather inhibits them.
Choice B is wrong because ANP is not stimulated to release when blood volume decreases, but when it increases.
ANP acts to reduce blood volume by promoting diuresis and natriuresis.
Choice C is wrong because ANP does not raise blood pressure, but lowers it. ANP acts as a vasodilator and reduces peripheral resistance.
Correct Answer is A
Explanation
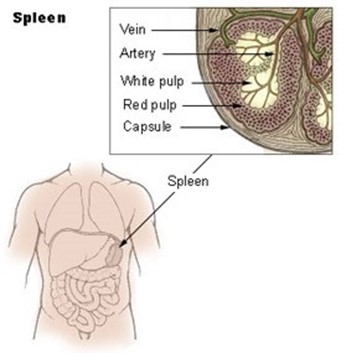
It is a major component of the lymphatic system and contains T and B lymphocytes.
Choice B is wrong because the spleen does not produce T lymphocytes, but rather stores them.
T lymphocytes are produced in the thymus.
Choice C is wrong because the spleen does not filter lymph, but rather blood. It traps bloodborne microbes and produces an immune response to them.
Choice D is wrong because the spleen consists of one lobe and is located in the upper left abdomen below the diaphragm.
The description in choice D matches the thymus, not the spleen.
The normal size of the spleen in adults is about 12 cm long, 8 cm broad, and 3-4 cm thick, weighing about 200 g.
The normal range of splenic index (the product of length, width, and thickness) is 120-480 cm.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
