Patient Data
The nurse educates the parents on post discharge care for the child.
What should the nurse include in post discharge care education? Select all that apply.
Monitor for fever
Give only clear liquids for several days
Avoid any kind of bath or shower
Keep a pressure dressing on the site for one week
Alert the physician if the site bleeds or swells
The child may take ibuprofen for pain
Correct Answer : A,E,F
Choice A reason: Monitoring for fever is essential after cardiac procedures like the one described. Fever can be a sign of infection, which is a risk following any invasive procedure. Normal body temperature ranges from 97°F (36.1°C) to 99°F (37.2°C) for a typical child, but it can be slightly lower in the morning and higher in the late afternoon and evening.
Choice B reason: There is no need to restrict the child to clear liquids for several days unless specifically instructed by the physician for a particular reason. After cardiac catheterization, patients are usually encouraged to resume their normal diet as tolerated to promote recovery unless there are other concerns that warrant dietary restrictions1.
Choice C reason: Avoiding baths or showers is generally recommended immediately after cardiac catheterization to prevent infection at the catheter insertion site. However, this restriction is usually only for a few days, not indefinitely. The site needs to be kept dry and clean until it has sufficiently healed.
Choice D reason: Keeping a pressure dressing on the site for one week is not typically necessary. The dressing is usually checked and changed by healthcare professionals, and the site is monitored for healing. The dressing may be removed after a certain period, often before one week, as long as there are no signs of bleeding or infection.
Choice E reason: Alerting the physician if the site bleeds or swells is crucial. Swelling or bleeding can indicate complications such as infection or hematoma formation. Parents should be instructed to look for any signs of abnormal discharge, redness, or increased pain, which could signify an infection.
Choice F reason: The child may take ibuprofen for pain, but it should be under the guidance of a physician. Ibuprofen is an NSAID that can help with pain and inflammation. However, it’s important to use the correct dosage and to ensure it doesn’t interfere with any other medications the child may be taking.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C","D"]
Explanation
The client has rested well throughout the night with a continuous positive airway pressure (CPAP) device in place. Sequential devices are in place for venous thromboembolism prevention. The client ambulated 100 yards (91 meters) last night and 200 yards (183 meters) this morning. She reports pain rating of 2 on 0 to 10 scale, located in the abdomen, described as aching. She has tolerated fluids throughout the night with no nausea or vomiting.
Assessment findings
- Neurological Alert and oriented times 4.
- Cardiovascular WNL.
- Respiratory WNL.
- Gastrointestinal/Genitourinary Voided twice throughout night, urine clear amber in appearance. Reports no dysuria. No bowel movement but the client is passing gas.
- Integumentary 4 abdominal incisions from laparoscopic procedure sealed with surgical glue. No drainage, redness, or edema present.
- Musculoskeletal Reported chronic knee pain. 5+ strength in bilateral upper extremities, 5+ strength in bilateral lower extremities.
Correct Answer is C
Explanation
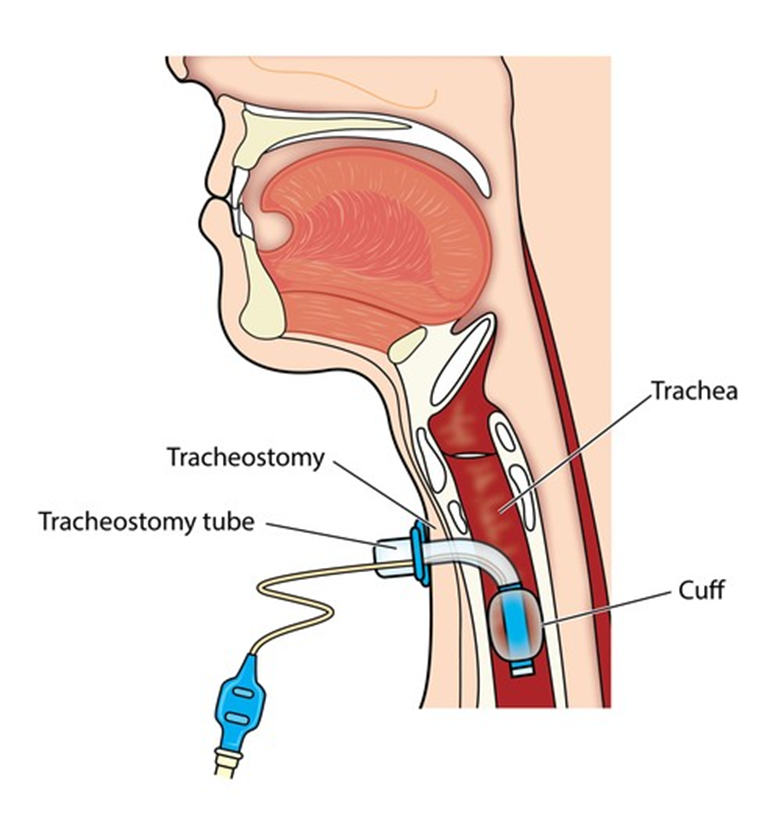
Choice A reason: Applying a water-soluble lubricant to the catheter is not recommended during tracheostomy suctioning as it may introduce contaminants.
Choice B reason: Instilling sodium chloride before suctioning is not a standard practice and can lead to complications such as edema.
Choice C reason: Wearing protective goggles is important to protect the nurse from potential splashes of bodily fluids during the suctioning process.
Choice D reason: Instructing the client to cough as the suction tip is removed is not recommended as it can cause discomfort and potential harm to the tracheal lining.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
