A nurse is caring for a client who is postoperative following an appendectomy.
Vital Signs
1800:
Temperature 98.4° F (36.8° C) Heart rate 104/min
Respiratory rate 22/min
Blood pressure 142/80 mm Hg
O2 saturation 97% on room air
1800:
Client alert and oriented x 4
Skin warm and dry
Lungs clear on auscultation
Bowel sounds hypoactive in all four quadrants Urine clear yellow
Incisional dressing clean and dry
Client reports pain as 6 on a scale of 0 to 10
1815:
Morphine administered as prescribed
2000:
Temperature 98.4° F (36.8° C) Heart rate 110/min Respiratory rate 24/min
Blood pressure 158/88 mm Hg O2 saturation 93% on room air
Which of the following 4 client findings should the nurse report to the provider?
Bowel sounds
Oxygen saturation
Nausea
Vomiting
Pain level
Heart rate
Incision characteristics
Lungs sounds
Correct Answer : B,D,E,F
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. This is an incorrect action. Inserting air in the tube and listening for gurgling sounds in the epigastric area is not a reliable method to confirm NG tube placement, as it can produce false-positive results due to air entering the stomach or intestines.
B. This is a correct action. Aspirating contents from the tube and verifying the pH level is a valid method to confirm NG tube placement, as gastric contents typically have a pH of less than 5.5, while intestinal or respiratory contents have a higher pH.
C. This is an incorrect action. Reviewing the medical record for previous x-ray verification of placement is not sufficient to confirm NG tube placement, as the tube can migrate or become dislodged after insertion. X-ray verification should be done initially and whenever there is doubt about the tube's position.
D. This is an incorrect action. Auscultating the lungs for adventitious breath sounds is not a specific method to confirm NG tube placement, as it can indicate other conditions such as pneumonia or pulmonary edema. It can also miss signs of respiratory complications due to NG tube misplacement, such as pneumothorax or bronchial obstruction.
Correct Answer is A
Explanation
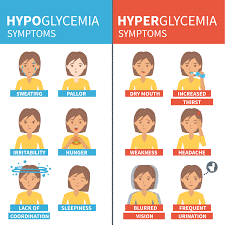
A. Irritability: Correct. Irritability is one of the signs of hypoglycemia, which occurs when blood glucose levels fall below 70 mg/dL (3.9 mmol/L). Other signs include shakiness, sweating, hunger, headache, confusion, and blurred vision.
B. Increased urination: Incorrect. Increased urination is one of the signs of hyperglycemia, which occurs when blood glucose levels rise above 180 mg/dL (10 mmol/L). Other signs include thirst, dry mouth, fatigue, nausea, and fruity breath odor.
C. Vomiting: Incorrect. Vomiting is not a specific sign of hypoglycemia or hyperglycemia, but it can occur as a complication of either condition if left untreated or poorly managed.
D.Facial flushing: Incorrect. Facial flushing is not a sign of hypoglycemia or hyperglycemia, but it can occur as a side effect of some medications used to treat diabetes, such as niacin or rosiglitazone.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
