A client with nasal congestion receives a prescription for phenylephrine 10 mg by mouth every 4 hours. Which client condition should the nurse report to the healthcare provider before administering the medication?
Diarrhea.
Bronchitis.
Hypertension.
Edema.
The Correct Answer is C
Choice A reason: Diarrhea is not a contraindication for phenylephrine, which is a decongestant that reduces swelling and mucus in the nasal passages. However, the nurse should monitor the client's fluid and electrolyte balance and provide adequate hydration.
Choice B reason: Bronchitis is not a contraindication for phenylephrine, which may help relieve some of the symptoms of bronchitis, such as nasal congestion and cough. However, the nurse should also encourage the client to use other measures, such as steam inhalation, expectorants, and rest.
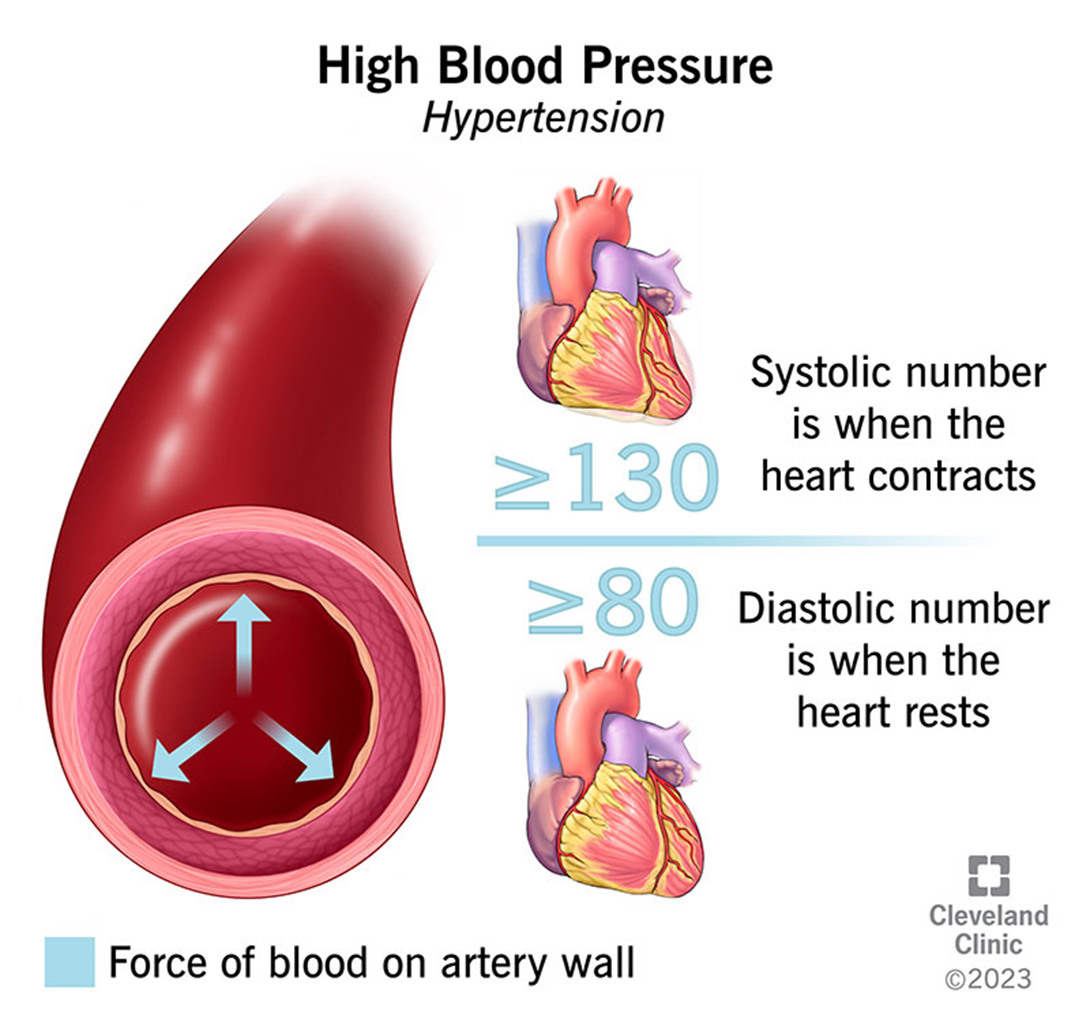
Choice C reason: Hypertension is a contraindication for phenylephrine, which can increase blood pressure and heart rate by constricting blood vessels. The nurse should report this condition to the healthcare provider and withhold the medication until further orders.
Choice D reason: Edema is not a contraindication for phenylephrine, which does not affect fluid retention or distribution. However, the nurse should assess the cause of edema and monitor the client's weight and urine output.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason: Notifying the healthcare provider of the carbamazepine level is the most appropriate action for the nurse to take. Carbamazepine is an anticonvulsant drug that requires close monitoring of its serum levels to ensure therapeutic and safe effects. The normal reference range for carbamazepine is 4 to 12 mcg/mL or 16.9 to 50.8 mmol/L. A level of 84 mcg/L (35.6 mmol/L) is significantly higher than the upper limit and indicates toxicity. The nurse should report this finding to the prescriber immediately and hold the dose until further instructions.
Choice B reason: Administering the carbamazepine as prescribed is not the most appropriate action for the nurse to take. Giving the evening dose of carbamazepine when the morning level is already toxic can worsen the client's condition and cause serious adverse effects, such as confusion, drowsiness, ataxia, nystagmus, or coma. The nurse should not administer the medication without consulting the prescriber.
Choice C reason: Assessing the client for side effects of carbamazepine is an important action for the nurse to take, but it is not the most appropriate one. The nurse should assess the client for signs and symptoms of carbamazepine toxicity, such as nausea, vomiting, headache, blurred vision, or seizures. However, this action alone is not sufficient to address the problem. The nurse should also notify the prescriber and withhold the dose.
Choice D reason: Withholding this dose of the carbamazepine is a necessary action for the nurse to take, but it is not the most appropriate one. The nurse should not give the evening dose of carbamazepine when the morning level is already toxic, as this can increase the risk of complications. However, this action alone is not enough to resolve the issue. The nurse should also notify the prescriber and follow the appropriate interventions.
Correct Answer is C
Explanation
Choice A reason: Providing a heating pad to the client may provide some temporary relief, but it does not address the underlying cause of the neck discomfort, which is likely due to extrapyramidal side effects (EPS) of the antipsychotic medication.
Choice B reason: Obtaining a prescription for physical therapy services may be beneficial for the client's overall health and well-being, but it is not the best intervention for the acute problem of neck discomfort. Physical therapy may also require a referral and a waiting period, which would delay the relief for the client.
Choice C reason: Giving a PRN prescription for benztropine is the best intervention for the nurse to implement, as benztropine is an anticholinergic medication that can counteract the EPS of the antipsychotic medication. Benztropine can reduce the muscle stiffness and spasms that cause the neck discomfort.
Choice D reason: Obtaining an extra pillow for the client to use at night may help the client sleep better, but it does not address the neck discomfort during the day. It also does not treat the EPS of the antipsychotic medication, which may worsen over time.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
