A nurse is monitoring a patient who is receiving a blood transfusion.
Which of the following symptoms should the nurse report to the charge nurse as a sign of an allergic blood transfusion reaction?
Bilateral flank pain.
Distended jugular veins.
Generalized urticaria.
Blood pressure 184/92 mm Hg.
The Correct Answer is C
Choice A rationale:
Bilateral flank pain is not a typical sign of an allergic blood transfusion reaction. It can be associated with other conditions, such as kidney problems, musculoskeletal issues, or abdominal aortic aneurysm. While it's important to assess flank pain, it doesn't directly suggest an allergic reaction to the transfusion.
Choice B Rationale:
Distended jugular veins can indicate fluid overload, which could potentially occur during a transfusion. However, it's not a specific sign of an allergic reaction. Fluid overload can result from various causes, including heart failure, kidney problems, or excessive fluid intake. It's crucial to monitor for fluid overload during transfusions, but it doesn't definitively point to an allergic reaction.
Choice C Rationale:
Generalized urticaria, or hives, is a hallmark sign of an allergic reaction. It's characterized by raised, red, itchy welts that can appear on various parts of the body. Hives can develop rapidly and spread extensively. During a blood transfusion, generalized urticaria strongly suggests that the patient's immune system is reacting to a component of the transfused blood, such as proteins or antibodies.

Choice D Rationale:
Blood pressure 184/92 mm Hg is elevated and could be concerning, but it's not specific to allergic reactions. High blood pressure can have various causes, including stress, pain, anxiety, or underlying hypertension. While monitoring blood pressure during transfusions is essential, it doesn't directly indicate an allergic reaction.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
The correct answer is choiceD.
Choice A rationale:
Assisting the client back into bed is not the initial action.Moving the client without assessing their condition could potentially cause harm.
Choice B rationale:
Notifying the client’s provider is important, but it should be done after assessing the client’s condition to provide accurate information.
Choice C rationale:
Informing the client’s family member is not the immediate priority.The nurse should first ensure the client’s safety and assess their condition.
Choice D rationale:
Obtaining the client’s vital signs is the initial action.This helps assess the client’s current condition and determine if there are any immediate medical needs.
Correct Answer is B
Explanation
Choice A rationale:
The spinal cord plays a crucial role in pain transmission, but it does not initiate the afferent pathways. It receives pain signals from nociceptors and relays them to the brain for processing.
The spinal cord is also involved in pain modulation, as it can dampen or amplify pain signals depending on various factors. However, it is not the primary trigger for pain sensation. That role belongs to nociceptors.
Choice B rationale:
Nociceptors are specialized sensory receptors that detect potentially damaging stimuli, such as intense heat, pressure, or chemical irritants.
They are located throughout the body, including the skin, muscles, joints, and internal organs.
When nociceptors are activated, they generate electrical signals that travel along nerve fibers to the spinal cord and brain. This process initiates the afferent pathways, which ultimately lead to the conscious perception of pain.
Nociceptors are essential for protecting the body from harm. They alert us to potential dangers and trigger responses that help us avoid injury or further damage.
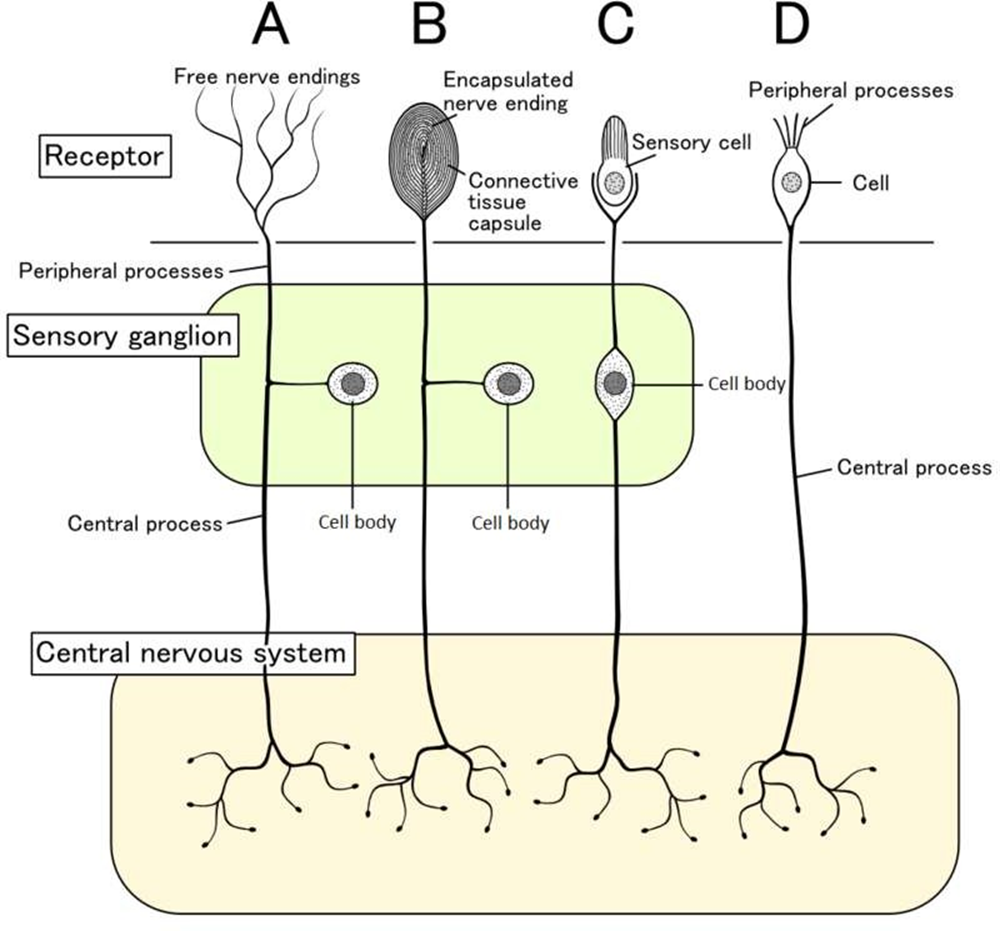
Choice C rationale:
Endorphins are natural pain-relieving substances produced by the body. They act on receptors in the brain and spinal cord to reduce pain perception.
However, endorphins do not trigger the afferent pathways. They work by modulating pain signals that have already been initiated by nociceptors.
Choice D rationale:
The cortex is the outer layer of the brain that is responsible for higher-level functions, such as thinking, feeling, and decision- making.
It plays a role in the conscious experience of pain, but it does not trigger the afferent pathways.
The cortex receives pain signals from the spinal cord and processes them, leading to the awareness of pain.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
