In which of the following types of pneumonia does consolidation involve the entire lobe of the lung?
Bronchopneumonia
Severe pneumonia
Empyema
Lobar pneumonia
The Correct Answer is D
Choice A Reason:
Bronchopneumonia is incorrect. Bronchopneumonia is characterized by patchy areas of consolidation involving multiple lobules scattered throughout the lungs. It typically results from bronchial obstruction and aspiration of infected material into the smaller airways and alveoli.
Choice B Reason:
Severe pneumonia is incorrect. "Severe pneumonia" is a broad term that can refer to pneumonia with various degrees of severity. It does not specifically describe the pattern of consolidation involving the entire lobe of the lung.
Choice C Reason:
Empyema is incorrect. Empyema refers to the accumulation of pus in the pleural cavity, often as a complication of pneumonia. It does not describe the pattern of consolidation within the lung tissue.
Choice D Reason:
Lobar pneumonia is correct. Lobar pneumonia is characterized by consolidation involving an entire lobe or lobes of the lung. It typically results from infection by a single pathogen, such as Streptococcus pneumoniae, which leads to inflammation and consolidation of an entire lobe of the lung.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
Depression is incorrect. While depression can contribute to headaches in some individuals, it is more commonly associated with migraine headaches rather than tension-type headaches or cluster headaches. People with depression may experience changes in neurotransmitter levels and alterations in pain perception, which can exacerbate migraines. However, tension-type headaches and cluster headaches are generally less strongly associated with depression as a precipitating factor compared to migraines.
Choice B Reason:
Smoking is incorrect. Smoking can be a trigger for headaches in some individuals, particularly migraines, due to the vasoconstrictive effects of nicotine and other compounds in tobacco smoke. However, smoking is not universally recognized as a common precipitating factor for tension-type headaches or cluster headaches. While individuals with cluster headaches may have higher rates of smoking compared to the general population, it is not a factor commonly shared with tension-type headaches.
Choice C Reason:
Poor posture is incorrect. Poor posture can contribute to muscle tension and cervical spine strain, which may trigger tension-type headaches. However, poor posture is not typically considered a precipitating factor specific to cluster headaches. While tension-type headaches may be exacerbated by poor posture, cluster headaches are characterized by severe, unilateral pain typically centered around the eye or temple, with associated autonomic symptoms such as tearing, nasal congestion, or ptosis.
Choice D Reason:
Stress is correct. Stress is a well-established precipitating factor for both tension-type headaches and cluster headaches. Stress can lead to muscle tension and contraction, which are common triggers for tension-type headaches. Additionally, stress can also contribute to the onset or worsening of cluster headaches, although the exact mechanisms underlying this association are not fully understood. Therefore, stress is a common precipitating factor for both tension-type headaches and cluster headaches.

Correct Answer is ["B","D","E"]
Explanation
Choice A Reason:
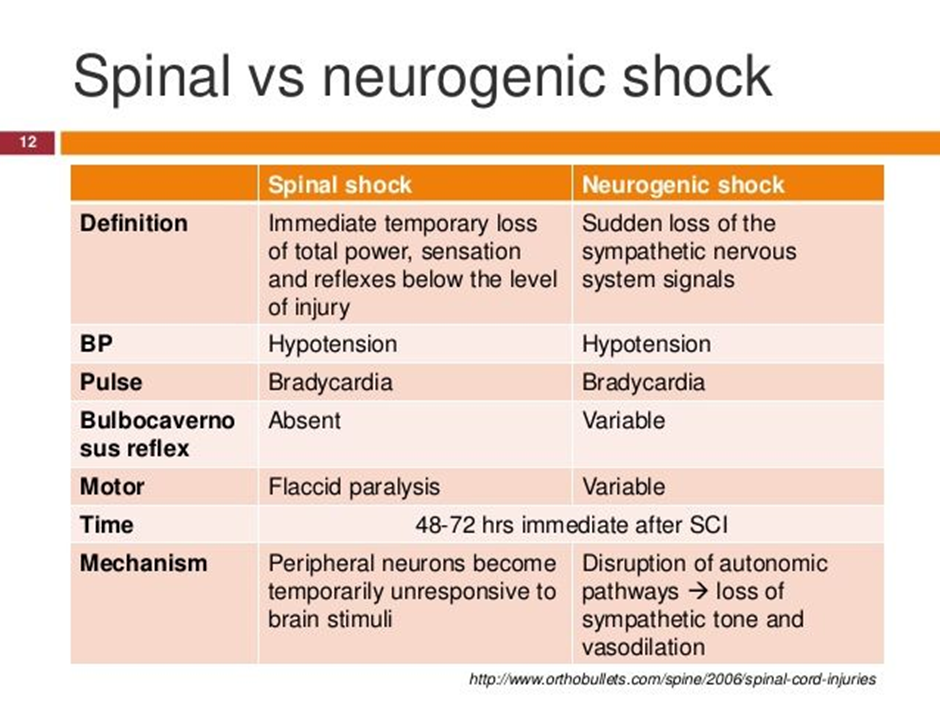
Metoprolol is incorrect. Metoprolol is a beta-blocker medication commonly used to treat conditions such as hypertension, angina, and heart failure. However, in the context of neurogenic shock following a spinal cord injury, the use of beta-blockers such as metoprolol is generally contraindicated. Beta-blockers antagonize the effects of sympathetic activation, leading to a reduction in heart rate and myocardial contractility, which can exacerbate hypotension and bradycardia, the hallmarks of neurogenic shock. Therefore, the nurse would not anticipate a prescription for metoprolol in the management of neurogenic shock.
Choice B Reason:
Lactated Ringers intravenous fluid is correct. Fluid resuscitation with isotonic crystalloid solutions such as lactated Ringers is essential to restore intravascular volume and improve perfusion.
Choice C Reason:
Furosemide is incorrect. Furosemide is a loop diuretic medication commonly used to treat conditions such as heart failure, edema, and hypertension by promoting diuresis and reducing fluid volume. However, in the context of neurogenic shock, the use of diuretics such as furosemide is generally not indicated unless there is concurrent volume overload. Neurogenic shock is characterized by hypotension due to vasodilation and decreased systemic vascular resistance, often leading to relative hypovolemia rather than volume overload. Therefore, administering furosemide could further decrease intravascular volume, exacerbating hypotension and compromising perfusion. As a result, the nurse would not anticipate a prescription for furosemide in the management of neurogenic shock.:
Choice D Reason:
Dopamine is correct. Dopamine is a vasopressor medication that acts to increase vascular tone and blood pressure by stimulating alpha-adrenergic receptors. It is commonly used in the management of neurogenic shock to augment blood pressure.
Choice E Reason:
Epinephrine is correct. Epinephrine is a potent vasopressor that acts on both alpha and beta-adrenergic receptors, leading to vasoconstriction and increased cardiac output. It is used in the treatment of refractory hypotension in neurogenic shock.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
