During a fecal impaction removal, an older client complains of feeling dizzy and cold.
Which intervention should the nurse implement?
Instruct the unlicensed assistive personnel (UAP) to apply a warm blanket and massage the client's back.
Insert a gloved finger into the rectum and gently massage the rectal sphincter.
Stop the procedure and observe for a reduction in symptoms before continuing.
Encourage the client to take slow, deep breaths while continuing the procedure.
Encourage the client to take slow, deep breaths while continuing the procedure.
The Correct Answer is A
Choice A rationale:
Instructing the UAP to apply a warm blanket and massage the client's back is the appropriate intervention in response to the client's complaints of feeling dizzy and cold during a fecal impaction removal procedure. These symptoms suggest a vasovagal response, which can be managed by keeping the client warm and providing comfort. This intervention helps increase blood flow and alleviate symptoms.
Choice B rationale:
Inserting a gloved finger into the rectum and massaging the rectal sphincter is not the first-line intervention when a client complains of feeling dizzy and cold during a fecal impaction removal. This invasive procedure should be reserved for cases where other interventions have failed, and it is necessary to complete the impaction removal.
Choice C rationale:
Stopping the procedure and observing for a reduction in symptoms before continuing is a reasonable approach, but it does not address the immediate discomfort and distress the client is experiencing. Providing comfort measures, such as applying a warm blanket and massaging the client's back, should be the initial response.
Choice D rationale:
Encouraging the client to take slow, deep breaths while continuing the procedure may not be effective in addressing the client's symptoms of dizziness and coldness. The client may require immediate comfort measures to stabilize their condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
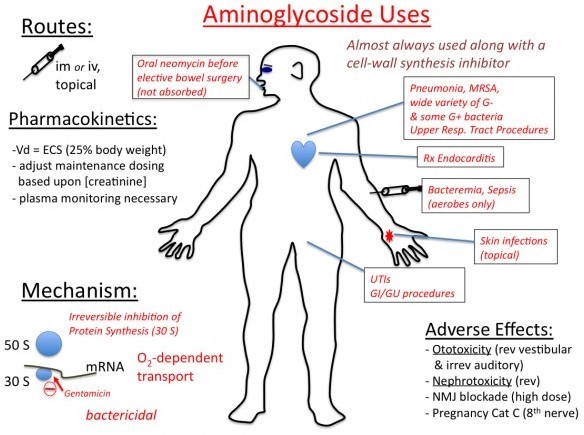
This is the correct answer because it is the best way to assess for signs of ototoxicity, which is a potential adverse effect of aminoglycosides. Ototoxicity is the damage or injury to the inner ear or auditory nerve caused by certain drugs or chemicals. It can result in hearing loss, tinnitus, vertigo, or balance problems. Aminoglycosides are a class of antibiotics that are effective against gram-negative bacteria, but they can also cause ototoxicity by interfering with the function of the hair cells in the cochlea. The practical nurse (PN) should monitor the client's hearing by asking about any changes in hearing acuity, ringing in the ears, or difficulty understanding speech. The PN should also perform a hearing test using a tuning fork or an audiometer if available. The PN should report any signs of ototoxicity to the health care provider and discontinue the aminoglycoside as ordered.
a) Check for changes in vision.
This is not the correct answer because it is not related to ototoxicity. Vision is the ability to see and perceive objects and colors using the eyes and the brain. Vision may be affected by various factors, such as age, genetics, eye diseases, injuries, infections, or medications. However, aminoglycosides do not cause vision problems or impairments. The PN should check for changes in vision in a client who is receiving other drugs that can cause ocular toxicity, such as ethambutol, chloroquine, or digoxin.
c) Observe the skin for a rash.
This is not the correct answer because it is not related to ototoxicity. A rash is a change in the color, texture, or appearance of the skin that may be caused by various factors, such as allergies, infections, inflammation, or medications. A rash may present as redness, itching, swelling, blisters, bumps, or scales.
Aminoglycosides can cause skin reactions such as rash or urticaria in some clients who are hypersensitive or allergic to them. The PN should observe the skin for a rash in a client who is receiving an aminoglycoside and report any signs of an allergic reaction to the health care provider. However, a rash is not a sign of ototoxicity.
d) Measure the urinary output.
This is not the correct answer because it is not related to ototoxicity. Urinary output is the amount of urine produced and excreted by the kidneys and bladder. It is an indicator of renal function and fluid balance. The normal range for urinary output is 0.5 to 1 mL/kg/hour for adults. Urinary output may be affected by various factors, such as fluid intake, dehydration, diuretics, kidney disease, or medications. Aminoglycosides can cause nephrotoxicity, which is another potential adverse effect of these drugs. Nephrotoxicity is the damage or injury to the kidneys caused by certain drugs or chemicals. It can impair the kidneys' ability to filter waste products from the blood, resulting in reduced urine production and oliguria. The PN should measure the urinary output in a client who is receiving an aminoglycoside and report any signs of nephrotoxicity to the health care provider. However, urinary output is not a sign of ototoxicity
Correct Answer is A
Explanation
The correct answer is choicea. Carry on with surgical preparation of the client without a signed informed consent.
Choice A rationale:
In emergency situations where immediate surgery is required to save a patient’s life and no family members are available, the doctrine of presumed consent applies.This means that healthcare providers can proceed with necessary treatment without a signed informed consent to prevent serious harm or death.
Choice B rationale:
Asking the man’s friend to sign the informed consent is not appropriate because friends are not legally authorized to provide consent for medical procedures unless they have legal documentation proving their authority.
Choice C rationale:
Notifying the unit manager for an emergency court order would delay the necessary surgery, which could be detrimental to the patient’s health. In emergencies, immediate action is required, and waiting for a court order is not feasible.
Choice D rationale:
Continuing to provide life support while searching for a guardian would also delay the necessary surgery. In life-threatening situations, immediate surgical intervention is prioritized over finding a legal guardian.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
