An older client who is agitated, dyspneic, orthopneic, and using accessory muscles to breathe is admitted for further treatment. Initial assessment includes a heart rate 128 beats/minute and irregular, respirations 38 breaths/minute, blood pressure 168/100 mmHg, wheezes and crackles in all lung fields. An hour after the administration of furosemide 60 mg IV, which assessments should the nurse obtain to determine the client's response to treatment? (Select all that apply.)
Skin elasticity.
Urinary output.
Oxygen saturation.
Lung sounds.
Pain scale.
Correct Answer : B,C,D
A. Skin elasticity:
Assessing skin elasticity is a measure of hydration status. Improved skin turgor may suggest that the client is responding positively to diuretic therapy by eliminating excess fluid. However, this may not be as immediate or specific as other indicators of response.
B. Urinary output:
Monitoring urinary output is crucial when administering diuretics like furosemide. Increased urine output indicates that the diuretic is promoting the elimination of excess fluid from the body, which is a desired effect in managing heart failure and fluid overload.
C. Oxygen saturation:
Assessing oxygen saturation is important in monitoring respiratory status. Improvement in oxygen saturation levels indicates that the client is responding to interventions aimed at relieving respiratory distress, such as the administration of furosemide.
D. Lung sounds:
Monitoring lung sounds is a key aspect of assessing respiratory function. Reduction in wheezes and crackles suggests that the diuretic is helping to alleviate pulmonary congestion and fluid accumulation in the lungs, contributing to improved respiratory function.
E. Pain scale:
Assessing pain is relevant if the client has reported chest pain or discomfort associated with heart failure. Reduction in pain may indicate improved cardiac function and response to treatment. However, it's important to note that pain assessment may not be as specific to the effects of furosemide as other respiratory and fluid status indicators.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Evaluate upper and lower extremities for perfusion, pulse volume, and pitting edema:
This option focuses on assessing perfusion and circulation in the extremities. While it's important in certain situations, in the context of a client who recently underwent cardiac stent placement and is now experiencing chest pressure and shortness of breath, the priority is to assess the cardiac status more directly.
B. Listen for extra heart sounds, murmurs, and rhythm with the bell of the stethoscope:
This option involves auscultating the heart for abnormal sounds or rhythms. While it's a valuable assessment in general, in this particular scenario, obtaining an electrocardiogram (ECG) and initiating continuous cardiac monitoring would provide a more comprehensive and immediate evaluation of the cardiac status.
C. Obtain a 12-lead electrocardiogram and begin continuous cardiac monitoring:
This is the correct choice. Obtaining a 12-lead ECG and initiating continuous cardiac monitoring is crucial in assessing the client's cardiac function. It allows for the detection of any acute changes in the heart's electrical activity or rhythm, which is essential for timely intervention and management.
D. Verify troponin level assessments are scheduled every 3-6 hours for a series of three:
Monitoring troponin levels is important in assessing cardiac damage, but in this acute situation, obtaining an immediate ECG and initiating continuous cardiac monitoring take precedence for a more real-time evaluation of the client's cardiac status. Troponin levels may be monitored subsequently based on the initial findings.
Correct Answer is B
Explanation
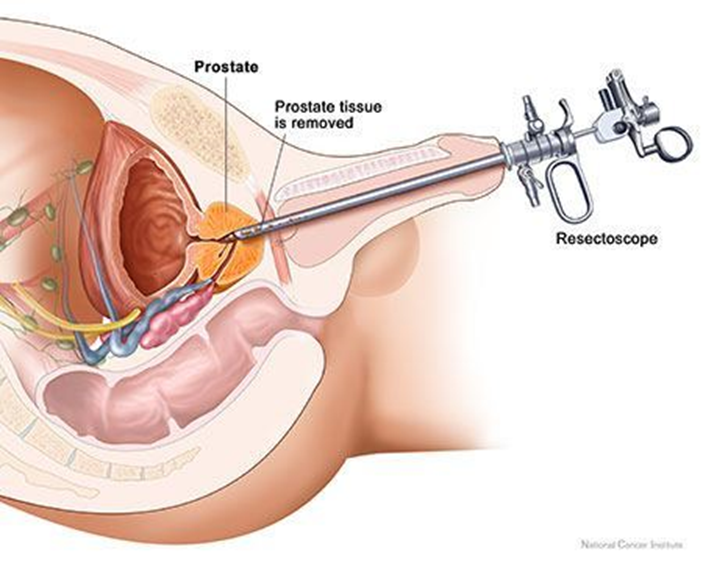
A. Irrigating the catheter manually:
Manually irrigating the catheter without an order may disrupt the clotting process and increase the risk of bleeding. It is not a routine nursing intervention post-TURP without specific orders.
B. Monitoring catheter drainage.
It is not within the nurse's scope of practice to manually irrigate the catheter without a healthcare provider's order, especially in the context of post-TURP care. The dark, pink-tinged outflow with blood clots indicates some expected bleeding following the procedure. The nurse should closely monitor the catheter drainage for the amount, color, and presence of clots.
C. Discontinuing infusing solution:
Discontinuing the normal saline irrigation may lead to clot formation and obstruction, potentially worsening the situation. The continuous bladder irrigation is often used to prevent clot formation and maintain catheter patency post-TURP.
D. Decreasing the flow rate:
The flow rate is typically set by the healthcare provider to maintain catheter patency and prevent clot formation. Decreasing the flow rate without specific orders may not be appropriate in this situation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
