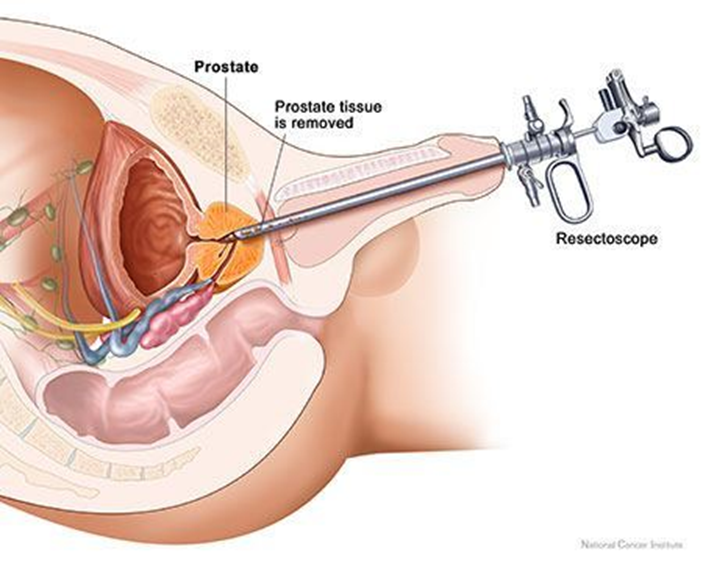
A client arrives to the medical-surgical unit 4 hours after a transurethral resection of the prostate. A triple-lumen catheter for continuous bladder irrigation with normal saline is infusing and the nurse observes dark, pink-tinged outflow with blood clots in the tubing and collection bag. Which action should the nurse take?
Irrigating the catheter manually.
Monitoring catheter drainage.
Discontinuing infusing solution.
Decreasing the flow rate.
The Correct Answer is B
A. Irrigating the catheter manually:
Manually irrigating the catheter without an order may disrupt the clotting process and increase the risk of bleeding. It is not a routine nursing intervention post-TURP without specific orders.
B. Monitoring catheter drainage.
It is not within the nurse's scope of practice to manually irrigate the catheter without a healthcare provider's order, especially in the context of post-TURP care. The dark, pink-tinged outflow with blood clots indicates some expected bleeding following the procedure. The nurse should closely monitor the catheter drainage for the amount, color, and presence of clots.
C. Discontinuing infusing solution:
Discontinuing the normal saline irrigation may lead to clot formation and obstruction, potentially worsening the situation. The continuous bladder irrigation is often used to prevent clot formation and maintain catheter patency post-TURP.
D. Decreasing the flow rate:
The flow rate is typically set by the healthcare provider to maintain catheter patency and prevent clot formation. Decreasing the flow rate without specific orders may not be appropriate in this situation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
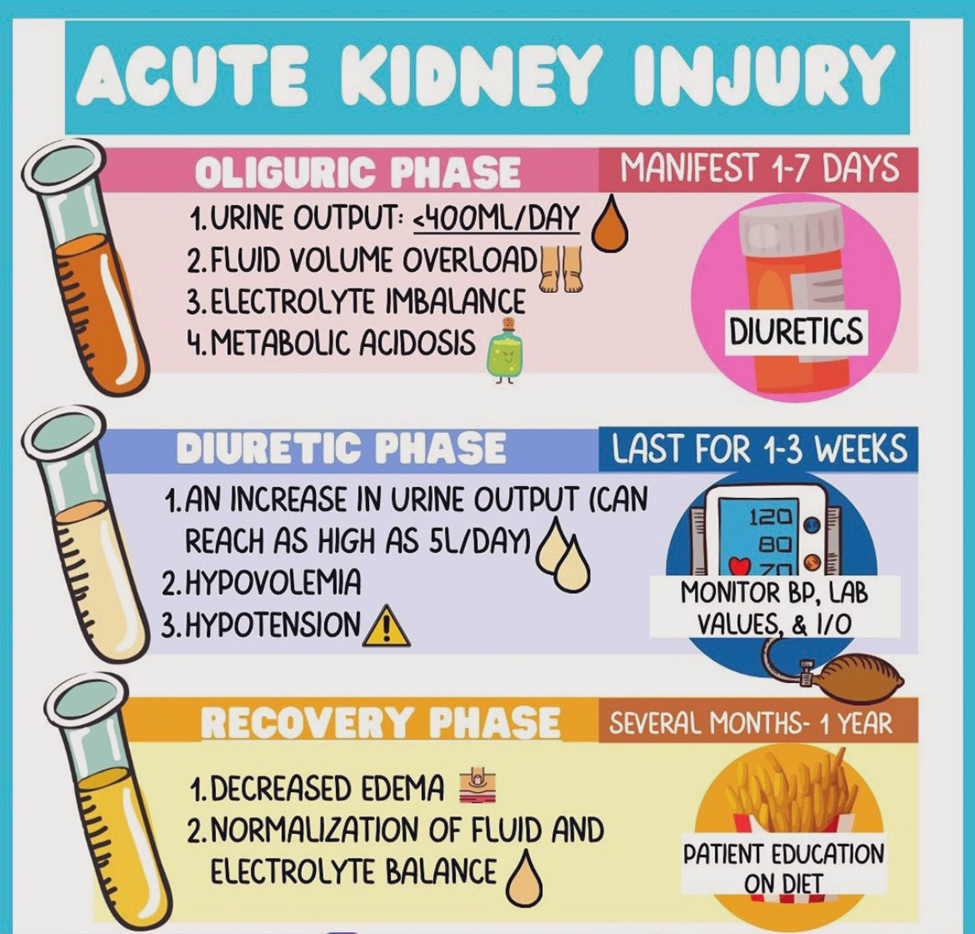
Correct Answer is A
Explanation
A. Hypovolemia and electrocardiographic (ECG) changes:
During the diuretic phase of AKI, there is an increased urine output, and the risk of dehydration and hypovolemia is elevated. The nurse should closely monitor fluid balance to prevent dehydration, and ECG changes may occur due to electrolyte imbalances (such as hypokalemia) associated with diuresis.
B. Uremic irritation of mucous membranes and skin surfaces:
Uremic symptoms are more prominent in the oliguric phase of AKI when waste products accumulate in the blood. In the diuretic phase, the focus shifts more toward managing fluid and electrolyte balance.
C. Side effects of total parental nutrition (TPN) and Intralipids:
TPN and Intralipids are not directly related to the diuretic phase of AKI. Monitoring for side effects of TPN and Intralipids may be relevant in other clinical contexts but is not the primary concern in the diuretic phase.
D. Elevated creatinine and blood urea nitrogen (BUN):
Monitoring creatinine and BUN levels is important for assessing kidney function, but in the diuretic phase, the focus shifts to managing fluid and electrolyte balance. The risk of hypovolemia and electrolyte imbalances is more immediate during this phase.
Correct Answer is D
Explanation
A. Remind the client to practice pelvic floor (Kegel) exercises regularly.
Pelvic floor exercises, such as Kegel exercises, are typically recommended for conditions involving weakened pelvic floor muscles. However, in the context of urinary retention related to sensorimotor deficits in multiple sclerosis, the issue is more neurological in nature. Therefore, pelvic floor exercises may not address the underlying problem effectively.
B. Provide a bedside commode for immediate use in the client's room.
While a bedside commode may be beneficial for individuals with mobility issues, it doesn't directly address the problem of urinary retention. It focuses on providing a convenient means for the client to void when needed, but it doesn't address the inability to empty the bladder spontaneously.
C. Explain the need to limit intake of oral fluids to reduce client discomfort.
Limiting oral fluids is not an appropriate intervention for urinary retention. In fact, it could lead to dehydration, which is not a recommended approach. The focus should be on addressing the difficulty in voiding through appropriate techniques.
D. Teach the client techniques for performing intermittent catheterization.
This is the correct choice. Intermittent catheterization is a direct and effective method to manage urinary retention in clients with sensorimotor deficits. Teaching the client how to perform intermittent catheterization empowers them to maintain regular bladder emptying and prevent complications associated with urinary retention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
