A wound care nurse has been consulted on a patient with multiple pressure wounds. The nurse comes across this heal wound. How should she document the following wound?
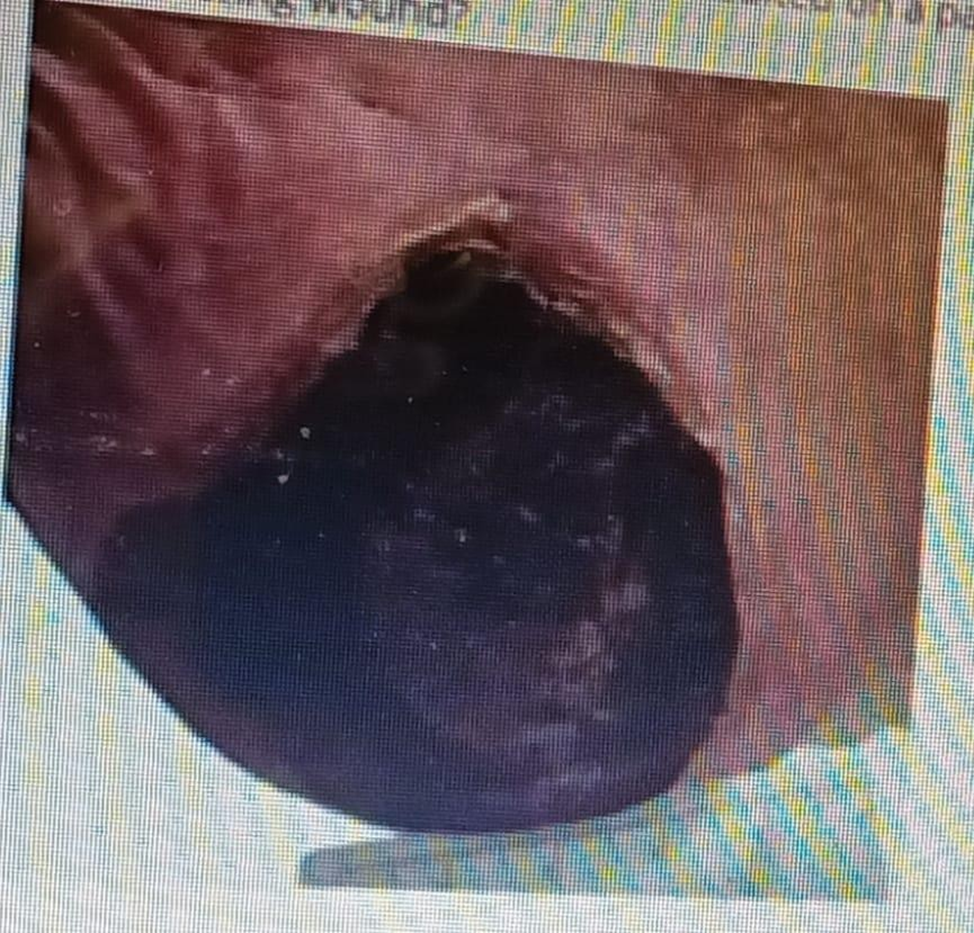
Unstageable Ulcer
Stage II Pressure Ulcer
Stage IV Pressure Ulcer
Stage III Pressure Ulcer
The Correct Answer is A
Choice A rationale: An unstageable ulcer is covered with slough or eschar, making it difficult to determine the depth of tissue involvement. The presence of eschar prevents accurate staging of the wound.
Choice B rationale: Stage II pressure ulcers involve partial-thickness skin loss, typically presenting as a shallow open ulcer with a red-pink wound bed.
Choice C rationale: Stage IV pressure ulcers involve full-thickness tissue loss with exposed bone, tendon, or muscle, which is not described in this scenario.
Choice D rationale: Stage III pressure ulcers involve full-thickness tissue loss without exposed bone, tendon, or muscle, but the presence of eschar makes accurate staging challenging.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale: Purulent drainage is thick and opaque, often indicating infection.
Choice B rationale: Serous drainage is thin and watery, typically clear or slightly yellow.
Choice C rationale: Sanguineous drainage is bright red and indicates fresh bleeding.
Choice D rationale: Serosanguineous drainage is thin and pale pink-yellow, representing a mixture of serous and sanguineous components.
Correct Answer is A
Explanation
Choice A rationale: An unstageable ulcer is covered with slough or eschar, making it difficult to determine the depth of tissue involvement. The presence of eschar prevents accurate staging of the wound.
Choice B rationale: Stage II pressure ulcers involve partial-thickness skin loss, typically presenting as a shallow open ulcer with a red-pink wound bed.
Choice C rationale: Stage IV pressure ulcers involve full-thickness tissue loss with exposed bone, tendon, or muscle, which is not described in this scenario.
Choice D rationale: Stage III pressure ulcers involve full-thickness tissue loss without exposed bone, tendon, or muscle, but the presence of eschar makes accurate staging challenging.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
